| "…I, like you, have seen how psychiatry has changed over the past 35 years I have been in practice. Over half of my practice are 15 min medication management appointments. I have learned to enjoy that as well as the psychotherapy I still do. There is a skill in med management and staying current is always a challenge. I remember when I was first out of training "poly pharmacy" was looked at askance, now it is the norm. To your suggestion. At both the summer and winter meeting usually have a lecture or two concerning pharmacology. By the design of the meetings, these are not meant to be all inclusive. I have found that the review courses such as offered by Harvard are the most useful. Web site is http://cme.hms.harvard.edu/cmeups/pdf/03124280.pdf." |
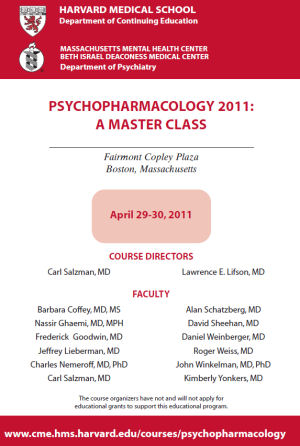
Earlier in the year, I wrote our Psychiatric Association about having seen or been called about many cases of misdiagnosed or mismanaged psychotropic drug withdrawal syndromes, suggesting a professional meeting with a theme like Psychotropic Drug Withdrawal Syndromes: Management and Treatment. What was on my mind was trying to help my colleagues be hyper-aware of the withdrawal states. My agenda was obviously to try to stop psychiatrists misinterpreting withdrawal states as increased or recurring illness and adding even more medication. Seemed like a reasonable thought. But I guess he thought I was asking for help for myself instead of suggesting that my colleagues needed the help. Oh well. But I clicked on the link anyway and it lead me to last year’s Master Pharmacology CME. This was the front of that Harvard brochure:
I remembered it from last year. A number of us wrote Dr. Salzman about it, asking why he had Nemeroff, Schatzberg, and Yonkers after their COI problems and investigation by the Senate [cme…]. He responded nicely assuring us there was no problem and the CME was being well received. So I thought I’d look at this year’s Psychopharmacology Master Class just to see what was up a year later:
For what it’s worth, Dr. Salzman seems to be going it alone this year – no other faculty listed. Maybe enrollment was down last year? or maybe the toxic former stars are finally losing their appeal?
That response at the top is from an old friend and a very decent guy. It’s typical – an acceptance of the way things are now for psychiatrists – not, I think, by choice. Comments like "Over half of my practice are 15 min medication management appointments. I have learned to enjoy that as well as the psychotherapy I still do. There is a skill in med management and staying current is always a challenge. I remember when I was first out of training ‘poly pharmacy’ was looked at askance, now it is the norm." are common when I run into people. My point is that when I come across old colleagues, they’re just doing what they do now – a lot of med checks. There’s no alarm, no sense that there are problems. It’s just the way it is. He recommended a CME and linked to one filled with discredited KOLs apparently unaware that he was doing that. He likewise missed the point of my letter which was pretty explicit – people aren’t so up on the drug withdrawal syndromes.

I am reading Cahill’s How the Irish Saved Civilization. In his chapter about how Rome fell and why, he includes this as one of the reasons:”the pretense that we still are what we once were.” He goes on to write:”the moral vocation of the man at the top to maintain order at all costs, while growing blind to the cruel dilemmas of ordinary life”. As Cahill asserts, these are lessons for the contemporary reader.
Great analogy…
BIG TIME Peggi. What you cite in the Rome example is basically a normalcy bias. This country (not just psychiatry) has it in a big way too. That is, everyone just plods along blindly, assuming “everything is under control” and that nothing is hugely wrong or abnormal.
I absolutely agree with Cahill that normalcy bias is one of the hidden factors of the decline of not just Rome, but other empires as well. There are still FAR too many psychiatrists who assume that “as long as my patients are fine, I’m fine. And psychiatry’s fine too.” It’s no different than a middle-class American thinking, “As long as I’ve still got my job and bennies, I’m fine. And America’s still fine too.”
But both the middle-class American and the psychiatrist don’t realize that the entire infrastructure is steadily collapsing around their ears and that one day it just may suck them into the vacuum too, and then they too will be out in the cold like us, wondering where all the good times went.
We ignore reality at our own peril…
That complacency is one reason I’m highly selective when it comes to psychiatrists — currently seeing one that is out-of-network for my insurer (and thus I have to effectively pay out of pocket for) and I’m happy to do it because he doesn’t do 15 minute med-checks, but really talks to me, and supports my desire to incorporate therapy and meds to deal with my depression (with maybe an eye towards reducing the meds if I can). I have found that this sort of psychiatrist is a rarity, sadly.
Interesting. I’ve just been going through Stephen Stahl’s oracular works. Although in his Prescriber’s Guide he tells clinicians to watch for withdrawal symptoms, he doesn’t describe them anywhere.
The assumption is doctors will know ’em when they see ’em.
Dr. Mickey, there are some psychiatrists and other doctors who are quite disturbed about the way things are going in the profession. Maybe not enough, yet, but it’s always a small group of dissidents who plant the seeds of change.
Perhaps when the doctors see the consumer revolt brewing….
On the other hand, I am told many doctors never see withdrawal reactions. That’s not on their radar as any kind problem. What to make of that?
Just curious, how many psychiatrist are behind the DSM-III?
and also, does the ICD-9 or -10 have the same problems as DSM-IV and -V?
A.L.
I never received training into rebound or withdrawal from psychotropics but I became familiar while taping down psychotropics in patients chronically exposed to medications.
Eventually I realized that we are confusing rebound symptoms with psychiatric symptoms and changing diagnosis in an attempt to make sense of the patients reactions. By using the DSM I was clearly convinced that it was not a psychiatric disorder morphing into another but something predictable and clearly related to decreasing psychotropics. The unbelievable resolution of all complaints after re-starting the psychotropic clearly pointed toward rebound no cinical manifestation of a disorder.
In my teaching of senior psychiatric residents I am focussing mostly on teaching rebound, drug interactions and side effects as well as avoidance of off label use of medication. They are not familiar with the content of my lecture and seems surprise of the wealth of knowledge i am providing, and how it makes sense.
It is fundamental to train psychiatric residents into this issueand hopefully we could remediate the problem over time. Most of the practicing psychiatrists were never trained and keep looking in the wrong place an explanation for patients’ symptoms, and it is the DSM. Same problem with substance abuser, we look for the DSM ignoring the exclusion criterias.