In 1886, Pliny Earle, then the superintendent of the state hospital for the insane in Northampton, Massachusetts, complained to his fellow psychiatrists that “in the present state of our knowledge, no classification of insanity can be erected upon a pathological basis.” Doctors in other specialties were using microscopes and chemical assays to discern the material causes of illness and to classify diseases accordingly. But psychiatrists, confronted with the impenetrable complexities of the brain, were “forced to fall back upon the symptomatology of the disease — the apparent mental condition, as judged from the outward manifestations.” The rest of medicine may have been galloping into modernity on the back of science, but Earle and his colleagues were being left in the dust…
But it’s not entirely clear that psychiatrists want a solution to the problem, at least not to judge from what happened when the experts conducting the most recent revision of the manual, the D.S.M.-5, were offered one. A group of seventeen prominent doctors — biological psychiatrists, experts in diagnostics, subspecialists in the field of depression, and even a historian — petitioned the D.S.M.-5’s mood-disorders committee to add a diagnosis they named melancholia…
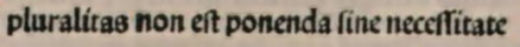
He is referring to the editorial, Whither Melancholia? in July 2010. Greenberg’s comment "a group of seventeen prominent doctors" is, if anything, an understatement. The list contains our brightest lights, cutting across ideologies and subspecialty politics. Were a council of elders ever assembled for psychiatry, it would be drawn from this list:
| Whither Melancholia? The Case for Its Classification as a Distinct Mood Disorder by Gordon Parker, M.D.; Max Fink, M.D.; Edward Shorter, Ph.D.; Michael Alan Taylor, M.D.; Hagop Akiskal, M.D.; German Berrios, M.D.; Tom Bolwig, M.D.; Walter A. Brown, M.D.; Bernard Carroll, M.B.B.S.; David Healy, M.D.; Donald F. Klein, M.D.; Athanasios Koukopoulos, M.D.; Robert Michels, M.D.; Joel Paris, M.D.; Robert T. Rubin, M.D.; Robert Spitzer, M.D.; & Conrad Swartz, M.D. American Journal of Psychiatry. 2010 167:745-747. [full text on-line] |
The editorial is brief, direct, and summarizes a definitive case for reinstituting Melancholia, our oldest and most clearly defined clinical syndrome – including the unique signs and symptoms, the well-defined biological markers, and the characteristic response to specific treatments. The editorial was ignored, but this New Yorker article adds something I hadn’t known – the DSM-5 Panel’s response:
“I believe you and your colleagues are fundamentally correct,” committee member William Coryell wrote to the melancholia advocates, by way of explaining his panel’s inaction. But “the inclusion of a biological measure would be very hard to sell to the mood group.” Coryell explained that the problem wasn’t the test’s reliability, which he thought was better than anything else in psychiatry. Rather, it was that the D.S.T. [Dexamethasone Suppression Test] would be “the only biological test for any diagnosis being considered.” A single disorder that met the scientific demands of the day, in other words, would only make the failure to meet them in the rest of the D.S.M. that much more glaring.
Coryell also noted that the melancholia proposal represented a departure from the notion, central to the D.S.M.’s descriptive method, that that the criteria for depression constitute a single disorder that every patient who matches the description has. “Depression is depression is depression,” another mood-disorders specialist has said, and so, Coryell counselled, evidence for such a “sweeping change” in paradigm would have to be “extensive and compelling.”
This notion — that the apparent mental condition is all that can matter — underlies not only the depression diagnosis but all of the D.S.M.’s categories. It may have been conceived as a stopgap, a way to bide time until the brain’s role in psychological suffering has been elucidated, but in the meantime, expert consensus about appearances has become the cornerstone of the profession, one that psychiatrists are reluctant to yank out, lest the entire edifice collapse.
So I would propose an alternative hypothesis for the behavior of the DSM-5 Task Force – maybe a parallel hypothesis. They wanted to be the new experts, the bright lights, the paradigm definers. They didn’t want to defer to any old guard, or previous leaders, or outside forces. It was their turn to shine, and the more advice they got, the further into their bunker they retreated. They took every suggestion, no matter how it was presented, as unreasonable criticism and said an intellectualized two year old "No." I doubt they were speaking for "psychiatrists" or even a paradigm, the group was caught up in a struggle and never got free. Things went badly – the wished-for biological underpinnings didn’t appear, McGorry’s early detection of Schizophrenia didn’t pan out, deadlines came and went, the Field Trials weren’t up to par, etc. Maybe if things had gone better, they might have been better listeners, but I doubt it. They came out of the gate determined to make their mark. And in a way, that’s exactly what they did.
Gary Greenberg mentions in his essay the potential of sleep EEG measures as biomarkers of melancholia. As it happens, it was David Kupfer, the chair of the DSM-5 task force, who developed this evidence in the 1970s and 1980s. To see him now ignore his own work is a cause of puzzlement.
I am one of the ‘gang of 17’ and several years ago I sent Dr. Kupfer materials addressing the use of biomarkers like his own in psychiatry. I did not receive a substantive response.
Having the power to determine what someone’s problem is while spending as little time as possible with that person, not having to think much about that person’s life and relationships, writing a prescription or combinations of prescriptions, seeing twenty patients in one day instead of five, and getting paid much more to do so; must be pretty heady. Why would a person enamored with their “expertise” and hooked on high pay for such low effort want to blow it all? As it is, psychiatrists get plenty of patients who suffer from an actual physical malady with psychiatric symptoms and can be paid to treat them like any other patient, because they are not much REQUIRED to look for or consider a physical cause in patients who don’t have a psychiatric disorder, much less those who do have one but aren’t responding to treatment.
Come to think of it, the lack of objective measure gives them special powers to see psychiatric maladies. Even though anyone can see their checklists, the psychiatrist has special powers to use it, so is granted a powerful subjectivity that can only be questioned by other psychiatrists who won’t.
So much of this kind of academic discussion is merely empire-building. Validity in patients is not relevant.