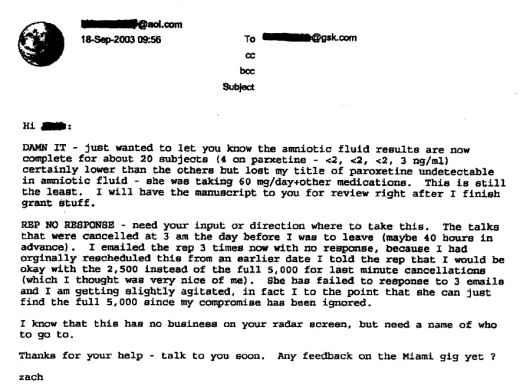
WSJBy DAVID ARMSTRONGJune 10, 2009Emory University has disciplined a prominent psychiatrist who was being paid by an antidepressant maker at the same time he was conducting federal research about the use of such drugs in pregnant women. The university said its medical school dean issued a letter of reprimand on April 30 to psychiatrist Zachary Stowe related to his "external relationships." Dr. Stowe was instructed to immediately eliminate conflicts related to current federal grants and was barred from having any conflicts for the next two years.
Dr. Stowe, the director of the Women’s Mental Health Program at Emory, is considered a leading expert on the use of antidepressants in pregnant women. He is listed as the primary investigator on at least three National Institutes of Health grants, beginning in 2003 and continuing through last year, that involve antidepressant use in pregnant women and the effects on children delivered by those women…
In a letter earlier this month to Emory, Sen. Charles Grassley (R., Iowa) said he learned the school had informed the NIH last summer that Dr. Stowe had financial conflicts of interest. The senator said records he obtained from GlaxoSmithKline PLC, the maker of the antidepressant Paxil, indicated Dr. Stowe was paid $154,400 by the drug company in 2007 and $99,300 during the first 10 months of 2008. The totals included payments for at least 95 promotional talks on behalf of the company. A Glaxo spokesman was unavailable for immediate comment…
We didn’t always think of experts as Key Opinion Leaders [KOLs]. Medical experts were physicians, usually academics, who devoted their interests and research to a particular aspect of the medical world. We went to their presentations and followed their writing and recommendations because they were the ones "in the know." Their centrality in medical opinion was earned at the bench and at the bedside. I have no idea when they became a commodity and went on the block. These days, the pharmaceutical companies have KOL managers that have meetings and journals. Zach Stowe was such a KOL – getting paid by drug companies to speak around the country. In fact, 5/7 authors on the paper were on multiple speaker’s bureaus. And the study was funded by the NIMH and two pharmaceutical companies.
by Anders Hviid, Mads Melbye, and Björn PasternakNew England Journal of Medicine. 2013 369:2406-2415.
Background: Studies have raised concern about an association between the use of selective serotonin reuptake inhibitors [SSRIs] during pregnancy and an increased risk of autism spectrum disorders in the offspring.Methods: We conducted a cohort study of all singleton live births in Denmark from 1996 through 2005 [626,875 births], with follow-up through 2009. Using Danish population registries, we linked information on maternal use of SSRIs before and during pregnancy, autism spectrum disorders diagnosed in the offspring, and a range of potential confounders. We used a survival analysis of the time to diagnosis in the offspring with Poisson regression to estimate rate ratios of autism spectrum disorders according to maternal use of SSRIs.Results: During 5,057,282 person-years of follow-up, we identified 3892 cases of autism spectrum disorder [incidence rate, 77.0 per 100,000 person-years]. A total of 52 cases during 42,400 person-years of follow-up involved offspring of women who were exposed to SSRIs during their pregnancy [incidence rate, 122.6 per 100,000 person-years]. As compared with no use of SSRIs both before and during pregnancy, use during pregnancy was not associated with a significantly increased risk of autism spectrum disorders [fully adjusted rate ratio, 1.20; 95% confidence interval [CI], 0.90 to 1.61]. Among women who received SSRIs before pregnancy but not during pregnancy, the corresponding fully adjusted rate ratio was 1.46 [95% CI, 1.17 to 1.81].Conclusions: We did not detect a significant association between maternal use of SSRIs during pregnancy and autism spectrum disorder in the offspring. On the basis of the upper boundary of the confidence interval, our study could not rule out a relative risk up to 1.61, and therefore the association warrants further study.[Funded by the Danish Health and Medicines Authority]
Pharmalotby Ed Silverman12/19/2013
Earlier this year, a study reported a link between antidepressants and autism, the second time in two years that such a relationship has been suggested. This week, a study in The New England Journal of Medicine found that children of women using SSRIs during pregnancy were not at increased risk of autism when compared with other children, although at the same time, the incidence of autism spectrum disorders in children born to women who used the drugs before pregnancy and then stopped was 46 percent than in other children. These results have fueled intensified debate over the extent to which there is cause-and-effect link. In the latest Pharmalot op-ed, Adam Urato, an assistant professor in the obstetrics and gynecology department at the School of Medicine at Tufts University, argues there is reason to be concerned that serotonin use that can alter the brains of developing babies…
I think this post tells a big story. These are good articles presenting an as yet unresolved issue – antidepressant use in pregnancy. Their sources are clean in so far as I can tell – addressing the medical issue rather than some drug company’s attempt at indication sprawl. They didn’t change my mind. I’m not going to be prescribing antidepressants or much of anything else to unborn babies, There are plenty of other ways to help depressed pregnant women. But my point is that this whole KOL era of the last several decades left us with the same questions it proposed to address, complicated by the biased literature of the period. The only way I found to negotiate those years was to be skeptical and conservative – relying on my own experience and that of colleagues I trusted. The usual resource of the literature at large had to be suspect and that was a difficult loss to deal with. That’s the way I see it – psychiatry’s lost years.
The post seems to imply that you cannot imagine individual circumstances where the severity of depression (currently or historically), and history of response to an SSRI so robust, that use of any SSRI use during that individual’s pregnancy could be warranted. Given your usual nuanced phrasing, especially when it comes to individualized clinical decision making between a patient and her physician, I’m not sure you meant I make such a blanket implication. It would seem that women who make a truly informed decision to continue certain medications during pregnancy (methadone comes to mind) already face enough stigma. This is NOT to imply that your overall point in the post increases such stigma. Not at all. But if something sounds more like a blanket statement it seems to run more of that risk. Keep up the good work
Annonymous,
Point taken and well made. It’s not quite as you say, but I wasn’t clear about it. Somewhere near “Do no harm,” I have another conviction. I’m not willing to become an arbitrary expert when I don’t know the right thing to do. In emergencies, one has to take the best shot, but I know of no situation where prescribing an antidepressant is ever an emergency. I don’t know what’s right to do here in the scenario you describe. And keeping up with the literature in this case hasn’t helped [which is the point of this post]. My felt reaction about medications in the first trimester is negative, but I don’t know that from either experience or study. I’m incapable of accurate risk/benefit assessment. In those situations, I find the best case true “expert” I can find and either get a consult or make a referral.
As physicians, much of what we do is [or becomes] intuitive. We can explain it if asked, but we did it automatically. It has become a schema. It’s useful to have flags on those schema, markers to say, put a stop to things and think this one through. The reason I mentioned that last case is that pregnancy is one of the places where I have such a flag. I don’t think the guy who put the patient on Depakote meant her harm. I know him, and he’s one of the good guys – a busy GP. And neither he nor she knew she was pregnant when he started it [though he didn’t stop it when he found out]. I’ve seen too many such cases to trust my intuition, and one of the reasons I know this particular literature is that I’ve looked at it more than once, and I haven’t trusted it either.
I have some areas of expertise too and saw a lot of consults in my practice. It’s a sign of a healthy medical community when that kind of thing happens. All I have is opinion in this case. That second conviction of mine has often been mentioned here. “The most important thing about being a doctor is knowing when you don’t know.” That’s one of the reasons we call the people we see “patients.”
Thanks for pointing that out.
That makes sense and helps clarify. Thank you very much for the thoughtful response.
If there’s a great deal of uncertainty about the effectiveness of an antidepressant for any woman, why subject a pregnant woman and her fetus to the risks?
There’s a basic assumption that, unlike every other type of drug known to exist, antidepressants are harmless, which deeply needs to be challenged across medicine.
Clearly, the broadening, over-diagnosing, and over-treatment of “depression” is a culprit and a gold mine. When I see a push to find a drug that can be made to appear harmless for pregnant women, I get the feeling that if the field could find a way to define 100% of any population “mentally ill” and drug them for life, they would. It appalls me that educated, intelligent people believe that 1 out of 4 people are mentally ill, that it’ s a biological conditions, and that anyone diagnosed with a mental illness should be on drugs. It’s manufactured madness.
Along with the notion that SSRI’s were safe in pregnancy , it was highly promoted that Untreated maternal depression was harmful to the fetus. This was not my area of focus but it was very similar to the notion that untreated psychosis is bad for the brain( in both cases treatment=drugs). Both concepts heighten the risks of taking a more cautious approach to prescribing. I know that the data on psychosis is suspect yet it took a strong hold on the field.
I agree, Sandra. Quite frequently, there are news articles about how “depression” (never consistently defined across studies) is associated with this physical illness or that.
These studies are all confounded by the fact that when people feel physically crummy, even though they might not have a diagnosable illness, they tend to feel down emotionally, too. There’s always a question about whether the illness caused the “depression” (a vague feeling something’s not right?) or vice versa.
Those who view everything through the lens of psychiatric diagnosis, a perspective that the general public has been encouraged by pharma propaganda to adopt, will see “depression” as the cause.
In pregnant women, a sense of isolation has been shown to be contributory towards pre- and post-natal depression. The proper therapy would be helping them establish a supportive social network, not further isolation with a psychiatric diagnosis and drug treatment that might harm the fetus.
You’d think that being doctors and all, that they’d want to study hormonal changes in women who are pregnant and who have just given birth, since women are obviously going through major hormonal changes during those times.
The topic you guys are onto is, in my mind, the most cynical of all the pharmaceutical misadventures in this era. It all had to do with “indication sprawl” and I think GSK was leading the pack. Paxil in adolescents [Keller et al]. Paxil in pregnancy [Stowe]. Paxil in physical illness [Nemeroff, Charney, etc.] What was remarkable was that it was essentially data free. There was a whole issue of biological psychiatry cheerleading treating depression in physically ill patients introduced by a Sally Laden special. [ought to be ashamed of themselves…]. Antidepressants are decidedly unhelpful in medically ill patients, but there are a lot of them so they went for the market. Pregnancy is right common too, so off they went. All of this hype solidified the notion that these drugs were “antidepressants” and any cause of “depression” required their use.
You betcha, Dr. Mickey.
Given that I see so many people (http://tinyurl.com/3o4k3j5) on absurd combinations of drugs for all kinds of ailments PLUS psychiatric drugs — with no doctor checking for drug interactions — I suspect physicians want to believe psychiatric drugs have no effects on the body overall and offhandedly throw them in to make the patient “feel better.”
PhRMA’s stealth message is that drugs like the atypical antipsychotic agents (Risperdal, Zyprexa, Geodon, Seroquel) are broad spectrum psychotropic agents, good for most of what ails you… analogous to the broad spectrum antibiotic drugs of the 1960s.
Seems antidepressants are a universal, one-size-fits-all answer for some doctors. Hubby (a long-time diabetic) had initial appointment with a new endocrinologist. Because lab work had not been completed, doc refused to address diabetes management or hypertension issues. But as he ushered hubby to the door, he handed him two FREE six-packs of seroquel. Diabetes obviously is a depressing illness that would somehow be bettered by daily consumption of an antidepressant??? Initial patient interview was also the final one. One wonders, though, how specialists from varied fields of medicine became expert (and so nonchalant) in administering antidepressant.
Melody,
And Seroquel isn’t an antidepressant, but an antipsychotic. Though that’s not your mistake. They got Seroquel CR® approved as an adjunct in depression, and I expect those handouts drugs came from some AstraZeneca detail man who visited that doctor. And that’s the real danger, drug reps having their way with general physicians. It’s the “broad spectrum” problem Dr. Carroll addressed above. Thanks for the story. It’s dead center on the problem.
http://www.bmj.com/content/347/bmj.f7140
Melody, Seroquel is an antipsychotic with a high risk of contributing to diabetes:
http://www.ncbi.nlm.nih.gov/pubmed/16943266
http://www.ncbi.nlm.nih.gov/pubmed/23278567
http://www.ncbi.nlm.nih.gov/pubmed/23106030
A very sloppy error. That endocrinologist should be replaced ASAP.
well.blogs.nytimes.com/2013/12/23/a-new-focus-on-depression/
Here is my take on that story… to the surprise of nobody, I am sure.
They did a sales switch on the link. Try this one.