N.I.M.H.By Thomas Insel and Pamela Hyde, SAMHSA AdministratorMay 1, 2014Conventional wisdom says that there is a long delay between a research finding and putting that finding into practice. Based on treatments for hypertension, that delay is usually described as 17 years. So it is especially worth noting an announcement last week from the Substance Abuse and Mental Health Services Administration [SAMHSA] that 5 percent of the Mental Health Block Grant allocation would be used to implement evidence-based treatments for first episode psychosis [FEP]. The overall approach – team-based, youth-oriented specialty care – was developed in consultation with the National Institute of Mental Health [NIMH], and is based on similar programs operating in Australia and Europe, as well as lessons learned in the Recovery After an Initial Schizophrenia Episode [RAISE] project. While part of the RAISE study is ongoing, completed studies in New York and Maryland have already demonstrated the feasibility of implementing this complex approach in community settings in the United States. Rather than a 17-year delay, the feasibility component of the RAISE project was completed in December, 2013, and is now being implemented by SAMHSA about 17 weeks later – a vast improvement in the timeline for moving research into real-world settings where it can truly have the broadest impact.
How did this happen so quickly? SAMHSA provides states funding via the Mental Health Block Grant to support local mental health programs. In this year’s budget, Congress directed SAMHSA to require that states set aside 5 percent of the Block Grant funds to support “evidence-based programs that address the needs of individuals with early serious mental illness, including psychotic disorders.” With recent experience demonstrating the feasibility of creating FEP treatment programs in U.S. community treatment settings NIMH staff developed an overview document for state planners and providers, Evidence-Based Treatments for First Episode Psychosis: Components of Coordinated Specialty Care [CSC], as well as a resources page that includes a variety of CSC program development materials, such as treatment manuals, videos, educational handouts, and worksheets. Like the interventions tested in the RAISE studies, CSC is based on collaborative treatment planning, a respectful and effective means for establishing a positive therapeutic alliance, and maintaining engagement with individuals and their family members over time.
To prepare states for the implementation of the set-aside, SAMHSA and NIMH are co-hosting national webinars to inform states of the evidence-based components of coordinated specialty care for FEP. In addition, SAMHSA will be providing technical assistance and resources to states as they develop and implement their plan. Some states already have significant investments to help individuals experiencing FEP. We encourage these states to coordinate existing programs with programs supported by the new 5 percent set-aside. We hope that, with this new Block Grant investment, leveraged by services reimbursed by Medicaid or private insurance, every state should be able to begin to develop or enhance early intervention services for FEP.
While SAMHSA’s mission is service and NIMH’s is research, we share the same goal of recovery for those experiencing a first episode of psychosis. Rather than a 17-year delay, this new announcement from SAMHSA uses the latest evidence to implement a much-needed innovation over the next few months across the country. This is a great example of what can happen when two agencies work together, moving research into practice to ensure the best outcomes.
This study, the RAISE Connection Program, is one of the two independent research studies that NIMH has funded to conduct the NIMH RAISE Project. The Connection Program is being supported in whole or in part with Federal funds from the American Recovery and Reinvestment Act of 2009 and the NIMH, National Institutes of Health, Department of Health and Human Services. The Connection Program aims to compare two early treatment interventions for adolescents and adults experiencing a first episode of psychosis. The study will also examine the costs associated with the treatment interventions…
This study will compare two different approaches to helping people get these treatments and services: a team-based approach versus a facilitated community-based approach. The study will determine if one of the approaches is better than the other in helping individuals go to work or to school, live independently, and have enjoyable relationships with others.
The Connection Program aims to to assess the effectiveness of a Team-based intervention for individuals with a first psychotic episode, observing outcomes over time for our study participants. When tracking outcomes, the Connection Program will make comparisons with what is known about the natural history of untreated first episode of psychosis as well as usual care outcomes from other experimental studies…
This study will adapt and evaluate the impact of a comprehensive and integrated treatment intervention for first episode psychosis to be delivered in real-world practice settings to promote symptomatic recovery, minimize disability, and maximize social, academic, and vocational functioning…
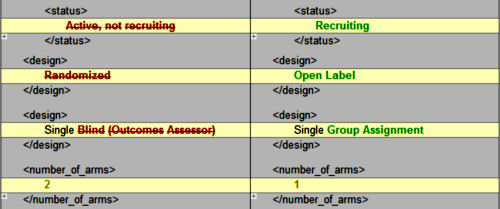
I read Dr. Insel’s blog post as something as a rah-rah-aren’t-we-swift-in-going-from-the-bench-to-the-bedside piece. But I was unclear about what it was that was being moved, so I looked it up on clinicaltrials.gov and looked at the history of changes almost out of habit. RAISE Connection started life as an uncontrolled comparative study, comparing two different intervention approaches in first break schizophrenic patients. Something happened [?], and it became a one-armed study with neither control or comparator, with a new recruitment period and a pared down enrollment. Dr. Insel presents it as a feasibility study.
The ETP study aims to compare two early treatment interventions for adolescents and adults experiencing a first episode of psychosis. The clinical centers have been randomly allocated to offer one of the two treatment programs. Both treatment interventions are designed to provide a person with treatment soon after he or she experiences the early signs of schizophrenia. Participants will be offered mental health services such as medication and psychosocial therapy. These strategies are all aimed at promoting symptom reduction and improving life functioning. Participation in this study will last between 2 and 3 years.
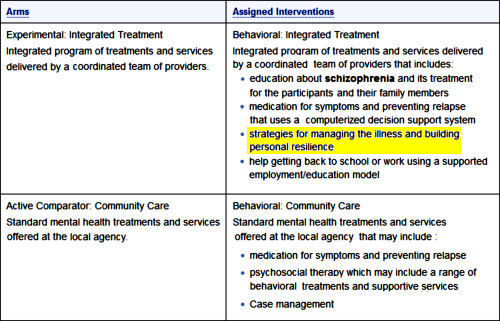
To rehash: The two "independent" RAISE studies were funded by the ARRA of 2009. The RAISE Connection study was at two sites [New York and Maryland] and was going to compare two different intervention programs in First Episode Schizophrenia. After a little over a year, the study was radically amended with a change in P.I., duration, enrollment target, and one intervention program dropped – meaning that there was neither control nor comparator. The outcome was to compare results with "…what is known about the natural history of untreated first episode of psychosis as well as usual care outcomes from other experimental studies." The study ended in December 2013 and I can find no published results. The RAISE ETP study was of similar design at 33 sites with a Mental Health Center treatment as usual arm and a Behavioral Integrative Treatment arm [see above].
In Dr. Insel’s version on his blog, the first study [RAISE Connection] is referred to as a feasibility study. The second study [RAISE ETP] is still continuing. So I’m having a difficult time understanding how this is an example of a "research finding and putting that finding into practice." Whatever happened to RAISE Connection removed any research from the field by eliminating any comparator. Even Dr. Insel referred to it as a feasibility exercise. The research study is RAISE ETP which has yet to be completed. They mention no preliminary results. So I just don’t get it.
You are right, Dr. Mickey. This is a breathtaking conceit by two Federal bureaucrats.
While your point is well taken, I must admit that I am glad there are some resources for psychosocial supports being directed to these Individuals and their families. There is reasonable data from other studies that support this general approach.