From January 1955 to December 1960, 269 patients who were considered among the most severely disabled and chronically mentally ill in the hospital were referred to the program. After the re-education of the staff, a program was constructed in collaboration with the patients that consisted of drug treatment, open-ward care in homelike conditions, group therapy, graded privileges, activity therapy, industrial therapy, vocational counseling, and self-help groups.
Obviously, the patients who were unable to live in the general community even with the wonder drug of the day, chronically psychotic, institutionalized, and without resources are a different population from the First Psychotic Episode cases addressed by the RAISE ETP program and targeted by its Individual Resiliency Training [IRT]. In reacting to the approach of RAISE, Dr. Steingard mentions the Open Dialog program in Finland as a program that includes the patient and family in the treatment process from the very beginning – a program that directly addresses the first episode patients. As I’ve read about Open Dialog, I’ve also been impressed and expect I’ll be reviewing it here shortly as well, but first I want to say something else that is one of the reasons I took the time to go back and review the Vermont story from the early days.
Dr. Brooks was an innovator who rallied his staff and patients around an approach that achieved something impressive. He put his most refractory cases on the new treatment [Thorazine] that helped 40% leave the back ward of the hospital. Buoyed by that success, he re-educated his staff and developed a program that was value added to the medication and helped many of the remaining non-responders move on to a much better life. It was a remarkable and enduring achievement. In fact, the Rhetoric associated with his program was exactly what I was taught as a psychiatric resident in 1974 when I started my training – the Rhetoric of the Community Mental Health Movement. I later even taught those very principles myself when I was on the faculty. But the Reality I saw was something very different. I saw chronic mental patients living under bridges and moving through what we called "revolving door" hospitalizations. Over the years, I saw "transinstutionalization" – the jails and prisons filling up with mental patients rather that the heroic successes of the Vermont experiment. I saw my friends in Public Mental Health "burning out" more quickly as centers and hospitals evaporated. And I saw anything that worked drowning under the weight of decreasing funds and an increasing case load. The Rhetoric/Reality gap has been consistent for the forty years I’ve been around.
When I look back at the Vermont studies, I question why some version of their program hasn’t been widely implemented for the last fifty years. The only part that really consistently stayed with us was the Thorazine [or some equivalent]. That’s what I saw in the 1970s and that’s what I see now. I would attribute that to several things. First, the Vermont program was initiated by Dr. Brooks and a staff that had fire in their bellies – they were on a mission. That’s a major factor in their success. And it was more or less time limited [outrunning burnout]. Second, Vermont is a homogeneous place – mostly rural or village/town based. Such a program is made for that kind of world. The Open Dialog program is in a similar location in Finland. Those communities tolerate chronically mentally ill people in a different way than urban environments. I live in such a place now, and can see that in my daily life away from the metropolis of Atlanta.
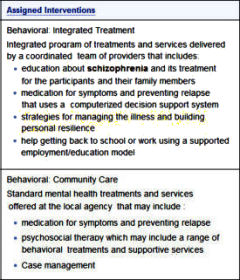 So when I look at the RAISE program and the push to implement it on a large scale, I think several things. I see nothing in the psychopharmacology manual that says what I want it to say – use antipsychotic medications only when you need to and the idea of using medications for life has long outlived any rational justification. The notion of using a computerized decision support system to medicate patients is unjustified by any science I know and antithetical to the principles of clinical medicine. The Individual Resiliency Training [IRT] Manual is paternalistic and not based on any understanding of the patients it’s designed to treat or the paths to the outcome being aimed for. Put it on the Internet along with the materials for any number of other approaches and let the individual programs figure out how they can best serve the clients they’re trying to help. Include what Dr. Brooks said, what’s happening with Open Dialog in Finland, etc. Develop another module to train the staff called "on being psychotic" developed by recovered patients and people who have spent their lives working among these patients – something designed to give new staff an acquaintance with the experience and difficulties involved in living with what has happened to their clients. And think about an ongoing staff project/meeting where people present their cases or things they’ve read about helping them. But most of all, do any and everything possible to help the staff develop the kind of "fire in the belly" that makes such programs actually work. Finally, adapt the program to the social and cultural environment where it’s being implemented. There will never be a one size fits all program.
So when I look at the RAISE program and the push to implement it on a large scale, I think several things. I see nothing in the psychopharmacology manual that says what I want it to say – use antipsychotic medications only when you need to and the idea of using medications for life has long outlived any rational justification. The notion of using a computerized decision support system to medicate patients is unjustified by any science I know and antithetical to the principles of clinical medicine. The Individual Resiliency Training [IRT] Manual is paternalistic and not based on any understanding of the patients it’s designed to treat or the paths to the outcome being aimed for. Put it on the Internet along with the materials for any number of other approaches and let the individual programs figure out how they can best serve the clients they’re trying to help. Include what Dr. Brooks said, what’s happening with Open Dialog in Finland, etc. Develop another module to train the staff called "on being psychotic" developed by recovered patients and people who have spent their lives working among these patients – something designed to give new staff an acquaintance with the experience and difficulties involved in living with what has happened to their clients. And think about an ongoing staff project/meeting where people present their cases or things they’ve read about helping them. But most of all, do any and everything possible to help the staff develop the kind of "fire in the belly" that makes such programs actually work. Finally, adapt the program to the social and cultural environment where it’s being implemented. There will never be a one size fits all program.
As I look at successful programs I see a common denominator of intense personal contact with a caring world, not a constant stream of medications. .Personal contact cost money, medications are cheap.
The legal system reacts after the fact and the cost are tremendous.
We really need to put the person back into the mental health discussion and the earlier the better.
Steve Lucas
In The Lancet a few weeks ago:
Chatterjee, S., Naik, S., John, S., Dabholkar, H., Balaji, M., Koschorke, M., … & Thornicroft, G. (2014). Effectiveness of a community-based intervention for people with schizophrenia and their caregivers in India (COPSI): a randomised controlled trial. The Lancet 383(9926), 1385-1394. Open access here.
(Much context about Sangath and its endeavors here.)
Quite interesting, partly because it’s written for lay ‘community health workers’, is COPSI’s A Manual for Working with People with Schizophrenia and their Families, linked (PDF) at the bottom of this page.
Nicely summarized, Dr. Mickey. At one level this story underlines George Engel’s construct of biopsychosocial approaches to aiding patients. Nowadays some self-styled critical psychiatrists like to contrast what they call a disease centered approach with a drug centered approach. Joanna Moncrieff in the U.K. is one of the proponents of the drug centered approach. Her dichotomy is a false dichotomy. What George Brooks in 1950s Vermont understood is that neither of Moncrieff’s models is right: it takes leverage on all 3 fronts to effect maximal help to a patient. In other words, Brooks understood that a person centered approach is needed. Beyond the Jasperian formality of the thought disorder, the content does matter – not for diagnosis but for treatment: it is what preoccupies the patient, after all. Your emphasis on the role of social setting in the expression of psychiatric illness also is well placed. That is an elementary principle of social medicine, which some of us learned in medical school years ago. To take a contemporary example, the experience of AIDS in Dar es Salaam is very different from what it is in San Francisco.
As you say yourself, there is a sense of déjà vu in reading about George Brooks and his work. How often do we need to reinvent the wheel? The disconnect between the early aspirations of comprehensive treatment for patients with psychosis and the later abject failures of the system is telling, but the lessons are administrative, not clinical or conceptual. And you are on target in emphasizing that Thorazine was a key ingredient in this history. Without Thorazine, George Brooks could not have reached first base. And he needed a lot more than Thorazine to make it to home base.
I guess I am a “self-styled critical psychiatrist” and I will explain why nothing in this work challenges Moncrieff’s construct and also why the disease model contributed to our blindness to the significance of this study. First of all, although I am a proponent of this sort of social intervention, I think the “biopsychosocial” construct allows us to continue with a simple reductionism without really admitting to it. I prefer thinking about this in layers (Kenneth Kendler had a nice article in AJP in which he articulates this much better than I will do here).
The biopsychosocial model, implies these things (biology/psychology/social) are fundamentally different and we therefore need different interventions to approach them. Alternatively, I would argue they are the same and we choose on which level we want to or can understand things. So there is a biological nature to psychosis (we are after all biological) but for some it may make more sense to understand and think about the psychosis on a social (traumatic experience, for example) and/or psychological (grief,loss) level.
Moncrieff argues that by assuming these drugs specifically target a disease, we convinced ourselves that we always (or at least almost always) needed the drug to treat that disease. It was not true in the 1950″s (when 2/3 of the patients did not improve with these drugs and were then enrolled in this program) and it is not true today. It also tends to blind us to the long term consequences of the drug because we are more inclined to consider long term decline as a part of the underlying disease state rather than a response to the drug. Over 70% of Harding’s subjects were recovered and not on drug or only taking them intermittently. People did not believe her data because it so challenged this disease model that by the 1980’s had been concretized in our field.
from Kendler:
http://journals.psychiatryonline.org/article.aspx?articleid=177378
See “Acceptance of explanatory pluralism”.
Sandra, the point of the biopsychosocial model is not to view the three elements as “fundamentally different.” And they are not “the same,” as you stated. The point of the model is to recognize that the three elements interact, both in the development of psychiatric disorders and in their resolution with treatment. The corollary is that you ignore any one of them at your peril – actually, at the patient’s peril.
As for Moncrieff’s critique of the disease model, it is filled with misinformation. She spends a lot of time critiquing her own straw man arguments. As just one example, there never was a class of drug called anti-schizophrenia that supposedly targeted the disease called schizophrenia specifically. From the get-go the neuroleptic or antipsychotic drugs were welcomed as clinically useful in a wide range of psychotic states – schizophrenia, yes, and also mania, and psychotic depression, and catatonia, and organic psychoses like Cushing disease, and acute delirium, and schizophreniform psychoses induced by drugs like amphetamine, and in the psychoses that can occur in temporal lobe epilepsy. Moncrieff notwithstanding, the claim of specificity for schizophrenia simply was never on the table.
I will just defer to the longer description by Moncrieff and Kendler. But Moncrieff does not claim these drugs weer promoted as anti-schizophrenia drugs but as anti-psychotics. She mainly argues that their effects of reducing psychotic symptoms is part of a larger impact they have on dopaminergic transmission. The point is that we might be better off just calling these drugs Dopaminergic blockers and then think about the broad implication of what that means. It may be helpful for some people at some time to reduce DA transmission but it comes at a cost that we need to fully understand. I just find this a useful way to think about this class of drugs. We label the SSRI’s in that fashion. Why not other drugs?
I keep wondering why no one is mentioning Loren Mosher’s work with Soteria House in the 60’s in these discussions. Those studies were done not on “back ward” people, but on young people with a first psychotic break. Treatment was social support provided mostly by non-degreed staff who interacted almost like peers. Medications were used minimally. There were controls—age and symptom matched people treated with usual inpatient treatment. The Soteria group was functioning better, with fewer relapses at (I think) 2 year follow up.
Does anyone know why this work gets as little publicity as it does? Are there design problems? I have always found them inspiring.
Dr. Combs,
There’s also Soteria Berne, ongoing. I can’t speak to the quality of the research, though.
Photos and a list of some publications here.
Another paper online here.
Video: Part 1, Part 2, Part 3
Sandra, it was you who said Moncrieff’s argument is that we assume these drugs specifically target a disease. Go work it out with her.
When you suggest relabeling antipsychotics as dopamine blockers, nothing is gained. Dopamine blockade and the many effects thereof have always been the subtexts concerning mechanism and safety in clinical use of the antipsychotic drugs. The label antipsychotic is just a way to communicate non-technically with patients.
Moncrieff’s drug-centered model of antipsychotic drug action is incoherent. She is on record as saying “Psychiatric drugs are psychoactive substances, like alcohol and heroin. Psychoactive substances modify the way the brain functions and by doing so produce alterations in thinking, feeling and behaviour. Psychoactive drugs exert their effects in anyone who takes them regardless of whether or not they have a mental condition. Different psychoactive substances produce different effects, however. The drug-centred model suggests that the psychoactive effects produced by some drugs can be useful therapeutically in some situations. They don’t do this in the way the disease-centred model suggests by normalising brain function. They do it by creating an abnormal or altered brain state that suppresses or replaces the manifestations of mental and behavioural problems.” Notice the poverty of content – airy assertions with no backup. Notice the hand waving repetition of the vague term psychoactive – it can mean anything at all. Notice the sleight of hand about medication effects in normal persons. What she says is correct for the side effects – but normal persons are not delusional and hallucinating, and the reversal of those features cannot be dismissed as just “a psychoactive effect.” That term explains nothing. In addition, normal subjects cannot even tolerate the chlorpromazine (Thorazine) equivalent doses that seriously psychotic patients require. Most normal subjects would sleep for 2 days if given 400-800 mg per day of chlorpromazine (and she wants to say there is no underlying abnormal state?). The antipsychotic effects in patients have no counterpart in the “alterations in thinking, feeling and behaviour” caused by antipsychotic drugs in normal subjects.
As a final irony, Moncrieff naively contrasts use of insulin for diabetes in the disease-centered model with use of alcohol for social anxiety in her preferred drug-centered model. She states “An accepted example of the drug centred model is the proposed benefits of alcohol in people who experience social phobia or social anxiety. Alcohol helps to reduce social anxiety not because it corrects an underlying biochemical imbalance, but because features of alcohol induced intoxication include relaxation and disinhibition. It is the superimposed state of intoxication itself that helps, not the effects of the drug on a disease mechanism.” First, there is no alcohol deficiency in social anxiety to match the undoubted insulin deficiency in Type I diabetes mellitus. Moncrieff’s argument here is quite specious. Moreover, alcohol is an agonist at GABA-A receptors in the brain. GABA is the primary inhibitory neurotransmitter in the nervous system, and activation of GABA-A receptors tends to decrease neuronal excitability. Current suggestions are that alcohol has this serendipitous effect in prefrontal-amygdala circuits, with associated lessening of anxiety. Moncrieff’s demand for evidence of “an underlying biochemical imbalance” is misplaced – it is a red herring argument. Certainly, the anxiolytic effect of one or two drinks cannot be conflated with a state of “intoxication.”
Dr. Carroll, thank you for your reply. Your point about alcohol in my mind supports her view. We think of alcohol as an intoxicant. Why not as an anxiolotyic? Why are the GABA effects in the prefrontal-amygdala circuits considered serendipitous? Because the drug was not developed in a lab to target those circuits? Then the neurloleptic effects were certainly serendipitous.
But this discussion, I sense, could go on forever, and goes beyond the scope of this place. As I said, I find her conceptualization helpful. I will leave it for others reading this exchange to go and read her latest book, “The Bitterest Pills” to form their own conclusions.
For anyone interested in a longer exposition of my own thoughts on this:
http://www.madinamerica.com/2013/11/diagnosis-disease-ilness/
(this is a version of my 1BOM guest blog).
The crucial issue of diagnosis is missing .these patients were diagnosed between 1955 and 1960 when there were no useful diagnostic standards. That they were considered schizophrenic or psychotic means nothing but “ought to be in a hospital” .The retrospective comparison with DSM3 Global assessment scale is wildly off a proper diagnostic comparison–which is almost certainly impossible. One should attend to
. Quitkin FM & Klein DF. Follow-up of treatment failure: Psychosis and character disorder. Am J Psychiatry 1967; 124: 499-505. Briefly, Hillside Hospital was for voluntary admissions. If you didn’t like the place you could pick up and go. However,certain patients were so disturbed and proclaimed active suicidality that simple discharge could not be tolerated, so they were committed to Creedmmoor State Hospital , almost all diagnosed schizophrenic. Over about ten years there were 60 such cases. I reviewed the quite good charts and relabeled 30 as non-psychotic character disorders. Fred Quitkin,blind to my rediagnoses , went to Creedmoor and was able to track down the outcomes . The 30 considered character disorders were discharged to the community in about 3 weeks . The schizophrenic group averaged 9 months and when discharged were simply considered non-dangerous if psychotic. It seems possible that the Vermont group included a substantial number of non psychotic patients ,mislabeled as was standard, who had much better prognoses ,and lack of need for anti-psychotics than chronic schizophrenics— where the relapse rate with drug discontinuation is high. This is not meant as a criticism of the program but of the probable misinterpretation of the data.
Sandra, of course the neuroleptic effects were serendipitous. So were the antidepressant effects and the anxiolytic effects. That is not news. What was your point?
Your position and Moncrieff’s on the alcohol example crystallizes our fundamental difference of perspective. The alcohol effect on anxiety, like all the other serendipitous discoveries from the 1940s through the 1960s, is important because it gives us a point of leverage into the mechanism of the disorder. In the case of alcohol, that point of leverage is activation of GABA-A receptors and inhibition of activity in brain circuits – we think prefrontal-amygdala circuits are the prime candidates. We don’t say alcohol or any other anxiolytic drug is correcting a chemical imbalance. We do say that the alcohol effect gives us a pharmacological target for developing safer anxiolytic agents than alcohol, and for eventually understanding the pathophysiology of the disorder. Moncrieff, on the other hand, doesn’t seem to grasp the distinction between pathophysiology and etiology. She is not satisfied with a pragmatic pharmacologic advance. She stridently demands evidence that psychiatric drugs reverse the root causes of disorders like anxiety, and in the absence of such complete evidence she declares that the drug’s action is irrelevant to disease mechanisms. That is a nonsequitur. Her alternative drug-centered model with its vague “psychoactive effect” has not yielded alternative points of leverage for understanding the disorder. But since she and her colleagues in the Critical Psychiatry Network don’t seem to accept the reality of diagnoses anyway, it is not surprising that they have to resort to a meaningless umbrella term like “psychoactive effect” to try to explain away what the drugs do. We can also note that most medications work at the pathophysiology level, not at the root cause level. Think anticonvulsants; think digoxin for cardiac failure; think antihypertensive drugs; think migraine treatments; on and on.
A final point: Moncrieff gives the impression that there is a professional dogma concerning the chemical imbalance theories of psychiatric disorders. Outside of corporate marketing, these are so yesterday. Among serious clinical scientists, excluding KOLs, the monoamine deficiency theories of depression, for instance, were already dismissed as simplistic as early as 1971, See PubMed ID#4936139. Regardless of what the irresponsible direct-to-consumer advertisements and the KOLs say about chemical imbalance theories, the American Psychiatric Association has never officially endorsed them. Just look in DSM-III through DSM-5.
p.s. Donald Klein makes some very cogent points in the previous comment.
Regarding Donald Klein’s comments; The second paper that Harding et al published in the AJP in 1987 was a a rigorous re-diagnosis by blind raters of the patients from the initial study. Dr. Brooks had kept extensive records since he had been conducting a study of Thorazine when it was first introduced. The raters used DSM III and looked at the outcomes of those who – using those criteria – still were diagnosed with Schizophrenia. The outcomes in the cohort were still good.
Regarding Dr. Carroll – although I agree that there is no professional dogma about the so-called chemical imbalance theory, I do find it interesting that in the NIMH’s own published manual for RAISE, they use the term chemical imbalance to explain schizophrenia. 1BOM cited that in a previous blog.
And yes, understanding what alcohol does in the brain gives us some understanding of how the brain works but it does not tell me that there is a condition called “anxiety” or, for that matter, social anxiety or generalized anxiety. Those terms are constructs we have created. They are not essential in the way I use that term above. In fact there are an abundance of states in which anxiety is an experience.
From “IRT, some comments”
“Speaking of honesty, again with this, of all groups, “honesty is the best only policy.” For example, on page 181 under Summary Points for – What is psychosis?, the manual includes:
Scientists believe psychosis is caused by a chemical imbalance in the brain.
Both stress and biology contribute to psychotic symptoms.
Biological factors contribute to this chemical imbalance in the brain.”
The re-diagnosis study:
http://www.ncbi.nlm.nih.gov/pubmed/3591992
Sandra, thanks for making my point for me. Insel is a KOL camp follower, and under Insel NIMH has no standing for pronouncements on dogma. The language some hacks inserted into the RAISE manual is irrelevant to the work of serious clinical scientists.