As with benzodiazepines in the 1980s, the UK is prescribing SSRI antidepressants at a staggering rate – and to no good effectThe Guardianby Peter Gøtzsche30 April 2014We appear to be in the midst of a psychiatric drug epidemic, just as we were when benzodiazepines [tranquilisers] were at their height in the late 1980s. The decline in their use after warnings about addiction led to a big increase in the use of the newer antidepressants, the SSRIs [selective serotonin re-uptake inhibitors]. Figures released by the Council for Evidence-based Psychiatry, which was set up to challenge many of the assumptions commonly made about modern psychiatry, show that more than 53m prescriptions for antidepressants were issued in 2013 in England alone. This is almost the equivalent of one for every man, woman and child and constitutes a 92% increase since 2003.
The problem is that many of these drugs simply do not work as people suppose. The main effect of antidepressants is not the reduction of depressive symptoms. They are no better than placebo for mild depression, only slightly better for moderate depression, and benefit only one out of 10 with severe depression. In around half of all patients, they cause sexual disturbances. The symptoms include decreased libido, delayed orgasm or ejaculation, no orgasm or ejaculation and erectile dysfunction. Studies in both humans and animals suggest that these effects may persist long after the drug has been discontinued. The US Food and Drug Administration has shown that antidepressants increase suicidal behaviour up to the age of 40, and many suicides have been reported even in healthy people who took the drugs for other reasons [for example, for stress or pain]. Another report also said that, among people over 65, antidepressants are believed to kill one out of every 28 people treated for one year, because they lead to falls and hip fractures. Indeed, it is not clear whether antidepressants are safe at any age.
My studies of the research literature in this whole area lead me to a very uncomfortable conclusion: the way we currently use psychiatric drugs is causing more harm than good. We should therefore use them much less, for shorter periods of time, and always with a plan for tapering off, to prevent people from being medicated for the rest of their lives.
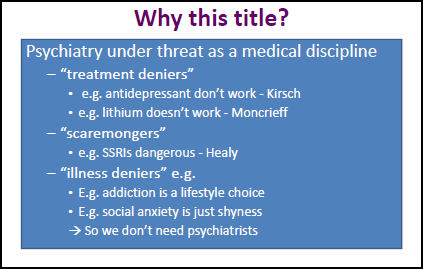
The Lancetby David J Nutt, Guy M Goodwin, Dinesh Bhuqra, Seena Fazel, and Stephen LawrieMay 27, 2014Psychiatry is used to being attacked by external parties with antidiagnosis and antitreatment agendas. However, the recent disclosure that a doctor [Professor Peter Getzsche] had joined a new group, the Council for Evidence-based Psychiatry, whose launch was accompanied by newspaper headlines such as "Antidepressants do more harm than good, research says" and "Psychiatric drugs are doing us more harm than good" in The Times and The Guardian plumbs a new nadir in irrational polemic. What is especially worrying is that this doctor is a co-founder of the Nordic Cochrane collaboration, an initiative set up to provide the best evidence for clinical practitioners. What is the truth about antidepressant efficacy and adverse effects, and why would Professor Getzsche apparently suspend his training in evidence analysis for popular polemic?
Of course, all active drugs have adverse effects, but for the new antidepressants these are rarely severe or life-threatening, even in overdose situations. Indeed, the new antidepressants, especially the selective serotonin reuptake inhibitors, are some of the safest drugs ever made. In our experience, the vast majority of patients who choose to stay on them do so because they improve their mood and well·being rather than because they cannot cope with withdrawal symptoms when they stop. Many of the extreme examples of adverse effects given by the opponents of antidepressants are both rare and sometimes sufficiently bizarre as to warrant the description of an unexplained medical symptom. To attribute extremely unusual or severe experiences to drugs that appear largely innocuous in double-blind clinical trials is to prefer anecdote to evidence. The incentive of litigation might also distort the presentation of some of the claims.
Whatever the reasons, extreme assertions such as those made by Prof Gøtzsche are insulting to the discipline of psychiatry and at some level express and reinforce stigma against mental illnesses and the people who have them. The medical profession must challenge these poorly thought-out negative claims by one of its own very vigorously.
Dr. Nutt’s reply to Dr. Gøtzsche is pretty much standard fare for him – forever championing the notion that there’s too much attention paid to adverse effects of the psychopharmacologic drugs. Three years ago, he made a similar speech to the Royal College of Psychiatry, No Psychiatry Without Psychopharmacology, that vilified Dr. David Healy as a "scaremonger" in an opening slide:
On the other hand, there are some things about this piece by Dr. Nutt that do bother me. In fact, most of what he writes bothers me. I think it dredges up my memories of the conflicts of the late 1970s. Dr. Szazs monotonous definitions of disease requiring some biological marker [the Myth of Mental Illness] and the neoKraepelinians going him even one step further by saying "The focus of psychiatric physicians should be on the biological aspects of illness" and then sliding over the years to Tom Insel’s "Psychiatry is a Clinical Neuroscience Discipline" version. I guess they all feel like dogmatic pronouncements or injunctions – but they’re really just opinions. I was personally comfortable with the more traditional Doctors take care of sick people. That’s who came to my office, and that’s what I did. Sickness came long before any biological understanding was around. We started with just "Do no Harm" and that’s where we’re still supposed to be. So my complaint is that besides Dr. Nutt’s pharmaphillia, and his neoKraepelinian bio-dogma, I think he perpetuates what seems to me a false dichotomy, one that goes back into the dawn of our history.
I don’t mind the characterization of political arguments like the typical antipsychiatry arguments for what they are. If a person has a confrontational style – it should not be surprising that they get confronted. There is nothing in the article by Nutt, et al that should be surprising. Any look at the pharmacoepidemiology and pharmacovigilance literature will support these arguments and I have posted several of this article on my blog.
The bias that I never see commented on is the extrapolation of clinical trials or meta-analyses to real life treatment scenarios. If it were true that antidepressants were only effective for 1 in 10 severe depressions there would really be no need to see psychiatrists or anyone else about depression. Nobody would ever leave a hospital. In fact the literature shows that more severe depressions are more likely to be associated with biological markers and not respond to placebos.
Are antidepressants overused? Probably as much as antibiotics, stimulants for ADHD, benzodiazepines, opioids, statins, H-2 blockers, and PPIs. Is there an advantage is over prescribing? Possibly in that antidepressant use in a national wide data base showed that they were associated with a decrease in suicide rate in the elderly.
Is the best solution to the problem a political one that relies heavily on rhetoric without a clear analysis of the problem and the solution. The answer to that is never. And I can think of clear precedents.
And don’t forget to look at all of the potential conflicts of interest. There are a lot more there than just on the part of the psychopharmacologists/biologists.
Once again, this Board-Certified-since-1975 psychiatrist agrees with everything you have said. Your blog validates my existence and my daily practice. Keep up the good work.
Again, the charge of overprescription is not based on those purportedly treated for Major Depressive Disorder so severe it requires hospitalization. It is aimed at the approximately 85% that do not have MDD or, indeed, any diagnosed psychiatric disorder (from CDC statistics). These people are subject to the adverse effects (and cost) with little benefit.
I do not understand how you continue to confuse this issue, Dr. Dawson.
The charge that critics of such overprescription are acting from bias against psychiatry is sheer ad hominem. I find it ironic that these prominent psychiatrists, who supposedly have been trained to parse motive in their patients to identify psychopathology, are prone to such erroneous reasoning. But that’s also true of their tendency to denial, which used to be considered an irrational defense mechanism.
A little detour perhaps, but this addresses the comment on stigma. I think that the psychiatrists proposing the “chemical imbalance” and need for medications have actually contributed to the stigma. When I tell my patients that my impression is that their depression arises not from some chemical imbalance but from their neuroendocrine response to the stresses that they have described to me, and that I will be using medications and therapy to help retrain their stress response system they usually express relief that there is not something inherently wrong with their brain.
So from my experience the overwhelming emphasis on inherent brain abnormalities causing mental illness has made the stigma worse and not less.
Would it be remiss of me, Dr. Arpaia to presume that you don’t take MEDICAID?
I cannot get away from the salesmanship nature of the Nut article. He paints himself as a victim, dismisses studies that do not support his position, and in a subtle way attacks his detractors.
This is a common theme in pharma where often we hear about the good people, fighting the good fight to improve people’s lives. We then follow on with the idea that these people work from some private bias, and nobody want to be bias, that people questioning these treatments are anti-patient.
Sales and psychiatry/psychology are very closely related. They do share one trait as pointed out by Dr. Gotzsche:
“Facts are the enemy of truth.”
In my sales management class of so many decades ago we were taught when confronting a salesperson to constantly rely on facts. Stay away from such ideas as “good people” “working hard” and avoid unsubstantiated concepts such as “everyone knows” or “people choose.”
This blog, along with a growing number of doctors, are taking that hard look at all of medicine and what they are finding is not pretty. That old concept of patient first has been perverted to me first. Leaders have often succumbed to the very traits they fight against.
Vilification of those we disagree with has become the norm and constructive debate has fallen to into the trash bin as subtle psychological attacks take center stage in an attempt to further a personal agenda.
Medicine long ago lost the whole concept of critical thinking as financial gain and personal glorification became the norm.
Steve Lucas
Here’s an unpleasant truth. Peer review is becoming a social club of academics and research has taken a nose dive. Here’s an example from another field:
http://www.washingtonpost.com/news/morning-mix/wp/2014/07/10/scholarly-journal-retracts-60-articles-smashes-peer-review-ring/
I’d have a lot more confidence in academic psychiatrists and research if they weren’t so collegial.
Corruption needs allies, and doesn’t need accountability or scrutiny.
Oh, catch at foxnews.com today’s little ditty about 90,000 people go to ERs for consequences with psych meds? Ambien is listed as the primary problem, but, when the hell did Ambien become a sole psych med?
$10 bet to the first one who honestly can confirm with a reliable source that Ambien is primarily written by psychiatrists. My bet is simply this: Ambien is written by non psych docs at least 70% of the time and then dumped on psych docs stupid enough to continue it more than 3 mos.
Oh, and why are sleep disorders assumed our domain with the prevalence of sleep disorder labs and specialists who are almost all NOT psychiatrists???
When do some of you finally have that “I’m mad as hell and won’t take this s–t anymore from idiots who aren’t psychiatrists who think they can do a better job as one!!!”
Unfortunately, the culture of academic psychiatry values menschiness and polity over honesty and good science. As Meehl pointed out, see what happens when you challenge someone at a case conference. Today, you get labeled antipsychiatry. What other branch of medicine puts up with this? Until the “key opinion leaders” of psychiatry put on their big boy pants, we will continue to be the ugly stepchild of medicine.
To Dr. Arpaia’s point – http://www.sciencedirect.com/science/article/pii/S0005796714000308