In the first decade of this century, there was a preoccupation with the idea that more efficacy could be extracted from these antidepressants. By the end of the decade, sequencing, augmenting, and combining had each failed to produce the dreamed of enhancement, and so for a time, researchers had a love affair with "personalized medicine" – coming up with some test that would predict response to one or the other antidepressants. It would seem like sequencing and combining would’ve answered that question, but apparently not. At the time, it was thought that genotyping would be the key [but anything would’ve done]. The Australian Brain Trainer, Evian Gordon, gathered one group of KOLs and began the iSPOT study. And Dr. Trevidi was funded for an NIMH study, EMBARC, to look for biomarkers that predicted drug response. His study started with Placebo, Citalopram [Celexa®], and Bupropion XL [Welbutrin XL®], but the Citalopram was replaced for unknown reasons with Sertraline [Zoloft®] not long after the study began. It was funded from September 30, 2010 through June 30, 2014. The NIMH web site has the following data available for funds allotted:
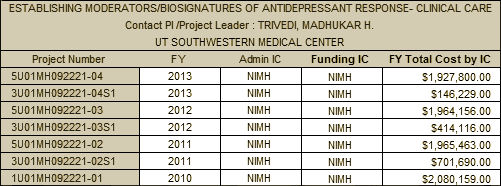
That comes to $9,199,613 so far. The overall cost to the NIMH for the four funded studies in the figure above [STAR*D, IMPACTS, CO-MED, and EMBARC] exceeds $50 M. Some time back, I had added a note to my calendar that EMBARC ended on June 30, 2014. My prediction was that it would not be completed – based on Dr. Trivedi’s poor track record and my own conviction that it wouldn’t show anything of any value just based on reading the protocol. While that cynical prediction remains an open question, the study should now be completed and yet it is still listed as "recruiting."
I doubt seriously that there’s anyone on the planet waiting to have a biomarker test to decide between Zoloft® and Welbutrin XL® for a depressed patient, particularly with a ~$10 M price-tag. TMAP was a scam; STAR*D was a bust; IMPACTS never even got off the ground. CO-MED flat-lined. Can EMBARC live up to that record? [I warned you I couldn’t contain the sarcasm]. It’s stories like this that account for my negativity about Dr. Insel’s NIMH. These people have been funded for a series of ill-conceived, badly designed, and poorly executed studies one after another for a decade and a half to the tune of $50 M. There’s just no need for that. STAR*D produced hundreds of forgettable papers, but never even really reported on what the study proposed to find out. Insel’s NIMH famously selects the directions for research rather than selecting from among the creativity of researchers own proposals. They chase things like personalized medicine, algorithmic medicine, measurement based medicine, translational medicine, RDoC, etc. – fads that come and go – and genomics, proteonomics, neuroimaging, connectomics – shiny objects that have appeared in view. And the same people get funded over and over, like the examples mentioned above, independent of their track records.
What do you think of this from GENDEP?
Study Finds That Common Lab Test Can Help Predict Antidepressant Treatment Response
I flagged that one, Arby. The article itself looks mighty shaky to me, but I’m going to look harder. First glance was thumbs down…
The name of the game is to keep the game going. For Insel’s NIMH bureaucracy, achieving excellent clinical science is incidental to that goal. That is why mediocrity prospers in the form of STAR*D and the rest. That’s why NIMH pandered to Charles Nemeroff and Dennis Charney, wasting millions on the stupidly conceived Emory-GlaxoSmithKline-NIMH Collaborative Mood Disorders Initiative 5U19MH069056 – an underperforming boondoggle if ever there was one.
When you talk about retiring the side I am reminded of what used to be said of the dominant psychoanalysts – that we would just have to wait for them to die off. Maybe the same is true for the present leaders of the academic-government-industrial complex.
With this spurious theory of “neuroprotection”, I think pharmaco-psychiatry has unleashed a plague that is wiping out sanity and patient-centered care all over medicine. The “vector” that spreads this infection is definitely the pharmaceutical industry. The concepts of meds-for-life and early-medication-for-patients-at-risk are now spreading to diabetes, weight loss, arthritis, you name it. It has nothing to do with any commonalities between the disease processes at issue, I’m convinced.
As readers of David Healy’s blog may know, I’ve been helping him dig into the marketing of Humira and other high-priced, risky biologic meds. I know very little about arthritis, Crohn’s disease, psoriasis or other conditions being targeted. But as a survivor of thirty years’ psychopharmacology I’ve been astonished at how utterly familiar the “medical” sales pitches sound:
1. This med must be taken for life — not just during flare-ups! That’s the only way to prevent further attacks. (We haven’t tested it beyond 3 months, BTW).
2. Improvement is not enough. We should medicate hard till we see Total Remission. Studies show that patients who don’t get completely “well” will have more episodes in the future. Besides, anything shy of Remission is selling patients short.
3. Meds once reserved for severe disease should actually be started early, at the first sign of disease. That way we’ll prevent it from ever becoming disabling. It’s, um, chondro-protective, or entero-protective, or something.
There is research being done to back all of this — but mostly it’s research that even a non-scientist reading Medscape can spot as shaky. I think it’s being designed in the marketing department and implemented in the clinic.
Has anyone else seen this? Wiley, I’d be real interested in knowing if you’ve spotted something like this among docs who treat MS.
Dammit! I’m a resident who just finished posting every TMAP algorithm I could find on my office desk’s pushpin board. I had (naively) thought they must be of some good clinical reference value…you really think it was all just a big push for pharma? I don’t see Lurasidone on there anywhere…
Anyway, would you apply the same harsh criticism to D. Osser’s work up at Harvard South Shore Psychiatry residency? (PubMed ID: 23656760).
If so, how should I go about studying then? The algorithms made things very streamlined.
For what it is worth, Patrick. I value David Osser’s work tremendously. I also respect his integrity. To the best of my knowledge, he has never taken pharma money. When we invited him to give grand rounds in Burlington, VT a few years ago, he insisted on taking the bus. He taught me psychopharmacology way back when and he has for many years carefully tracked the literature and tried to apply it in a systematic way.
I would be interested in Mickey’s view point but I do not think we need to dismiss algorithms completely. In some way, it is inherent to my work and it is good to make it explicit about how one thinks. For instance, one has a framework to decide whether to recommend a drug and then one needs to decide which one to pick. If that is not effective, we need to decide how long to wait before reaching that conclusion, what is the optimal dose, and whether it is worth switching to another drug.
Dr. Osser gave a talk called something like “cost effective approach to using drugs” so that alone gives you some idea of how he thinks. This was probably 10 years ago well before it became fashionable to think in those terms. At my clinic we have used this as a quality review. He made several points – do not use more than one antipsychotic, when to recommend clozapine, when to consider hypnotics, etc (I am happy to make this available to anyone) and we use this to review one another’s charts. It is a qualitative review and together we discuss the challenges in each individual situation.
The problem I see with these large scale studies is that the decisions become so complex that it is hard to evaluate them. What I think Osser does is to give a guide about clinical decision making that offers a nice balance between considerations of the individual sitting in the room and the data that is available to us. I think of it more as a guide than an algorithm.
Of course, neither Dr. Osser or anyone else can compensate for the fact that the literature is flawed in such a fundamental way due to publication bias, the bias of study design, etc.
You can contact me if you want more information on what we do.
Tacit knowledge is knowledge that cannot be fully communicated with words. The patient’s experience of mood is tacit knowledge. While that experience cannot be communicated with words if a clinician listens with enough time and empathy they can get a close enough approximation to figure out something helpful
Algorithms however require numbers, and if words cannot describe tacit knowledge, numbers are far worse. So to the extent we use algorithms as a substitute for listening the worse we do clinically.
There is nothing inherently wrong with an algorithm. But it can be hard to resist the temptation to use it instead of listening, especially when there is so much pressure to see patients faster.
When algorithms are taught as standards of care, which I am sure residency programs do, then how can you attack them from a legal perspective at the end of the day? Because, you can’t shame and humiliate the authors of these biased and unobjective plans, so if you want them dumped into the scrap heap, you have to make it a legal matter. Lawsuits and loss of profit is how you impact on leadership, whether it be the APA or institutional academia.
So, how do you poke holes in the premise to these algorithms? Find the paper trail, white or green, and keep back tracking until you find the bribery source? Ah, but as a wise physician/lawyer noted 15 years ago, the only way to get to the source of malfeasance and frank criminality is to have ignorant, stupid doctors be complicit and follow the advice/direction of non physician standards of care and then have negative outcomes occur.Then, let the “Discovery” process work its magic.
But that takes years, and people will have risk of morbidity and mortality. So, I guess we are back to shame and humility? With the jokers we have “leading” psychiatry at the moment, you’d have better luck negotiating with Assad, Putin, or Hamas. Hmm, seems to be the same type of personality disorder at hand here with the profession?
But, let’s keep debating, how far is retirement for some here?
Hi, Johanna. Copaxone is working for me and doing wonders. It really does need to be taken regularly and for life in order to provide the benefits of having longer remissions and slower progress of the disease.My gait has been normal all year, and I’ve just started having mild relapse, which is nothing to write home about.
What mildly surprises me lately is the discovery that even according to a meta-analysis done at the Oregon Health Sciences University there is no reason for baclofen to be a first line treatment for the muscle spasm of MS. There is simply no reliable evidence to back that up. My neurologist is an intern who works for OHSU and the Veteran’s hospital— the two hospitals are attached physically and operationally. The last time I saw him, I was in the throes of baclofen withdrawal and possibly oxycodone. He was clearly worried that I might be psychotic and didn’t recognize, even when I told him, the symptoms of baclofen withdrawal. I had been prescribed 10 mg 3 x daily, but had only been taking it twice daily for about a year. I took 10 weeks to wean off it and still had major withdrawal symptoms. Now I know what debilitating ADHD fees like, and have learned that most of what I thought was the physical, mental and psychological deterioration of MS, was actually the effects of baclofen; which included agnosia, depersonalization, serious memory impairment, sensory distortion so bad that it was painful to hear music, taste perversion, fatigue, sleep difficulties and disruption, near stupor with unbelievable stupidity, reduced motor control, and increased muscle spasm.
Coming out of all that was overwhelming to my senses which had been going into an increasingly deep hibernation, for years. It’s over now.
Hurrah!
Fortunately for me, I am nothing if not resilient and treated the hyperthermia with its dehydration myself for three days with a lot of Gatorade, spring water, and fresh juices. Since I did a lot of research before deciding to cut baclofen out first (and what luck!) I expected the hallucinations and so watched them with indifference. On the fourth day I ate and enjoyed it like I haven’t in three years. I’m also a good sport, play the hand that’s dealt me, and am thrilled to be back as the high-functioning person I;ve always been. I am able to do things now that I’ve wanted to do for a long time. I relish it.
Am tapering very slowly off amitriptyline now, which is routinely prescribed for MS pain without the fun fact that it only works for one out of three patients. It stopped making me sleepy a long time ago and I hadn’t been able to tell if it helped with the pain, but hormone replacements eliminated 95% of the horrible symphony of pains and unreal sensations throughout most of my body. Victory! The agnosia and depersonalization, I suppose, kept me from feeling like my life was going to be nothing but downhill with increasingly horrible pain from now on. I had feelings of resignation that only drug induced stupor can provide. Mixed blessings, I suppose.
Am still taking trazodone for sleep, but that’s the last med on my list to stop taking daily, and since sleep deprivation is brutal for me, I’ll keep some on hand to use as needed.
I’ve fallen for two prescribing cascades now— one for a disease I don’t have and one I most definitely do. It’s unnecessary pain and suffering either way and I think I’ve learned enough to embrace the wisdom of refusing most meds, the way I’ve refused Ativan. It can cause permanent muscle cramp and permanent memory impairment for an NNT of 500 and would mimic MS. I’m going to refuse mammograms from now on, as well. I’ve gotten plenty of radiation from my jobs with the Air Force and am disinclined to join in the “preventive medicine” frenzy.
I still have a report to finish for everyone on my primary care team and I’ll insist that they put it in my records. My high regard for epidemiology requires me to do so— as a veteran, my information is available for studies. I want to tell the world of women with MS about the hormone replacements— what a gift that is.
Am seeing a psyche nurse next week who is very helpful and knowledgeable when it comes to side effects and she wholeheartedly encourages minimal to no drug use. She doesn’t think that I’m bipolar and impossibly treatment resistant either. She prescribed guanfacine for my “ADHD” and it’s great. It works. I’ll take it because it works and is qualitatively superior to ritalin.
… amitriptyline only works for one out of four patients for nerve pain from MS….
Patrick,
I doubt there’s a doctor alive who doesn’t have a head filled with algorithms. I sure do. As a medical student and house officer, I had what we called an “ectopic Brain” with pages of algorithms and cut out charts to get me through the scary days. And as a chief resident, I wrote them myself for the new residents in my Internal Medicine Residency, and again in my second residency in Psychiatry. In training when everything is new, they help keep one from shooting from the hip. I noticed that the further along I got, the less often I opened that big little book, but I don’t recall being disenchanted with guidelines and algorithms until I got out and was practicing Internal Medicine.
The American Heart Association, the American Diabetic Association, etc. began to put out guidelines that were increasingly stringent and when I tried to use them, I made some people sick – actually more than some. Too many insulin reactions. Too many side effects from the antihypertensives of the day. And I came to see guidelines as recipes for some hypothetical median patient, or some patient the guidelines framers wanted my patients to be. My job was to see them as only a starting place, and find the best fit for the patient in front of me.
I wish I could say that for TMAP. Put TMAP in the search box on this blog, and the more you read, the more you’ll see is that the science behind those algorithms isn’t taught in medical school. A lot of it would be better taught in Marketing 101. So of course I’m not preaching against algorithms and guidelines. We have to have them. The sermon here is what Sandra says in the next comment. Even at your stage of training, I’d advise vetting the source and the motives of the guidelines framers with particular attention to Conflicts of Interest. It’s a conduit that has unfortunately been heavily exploited by industry, making it hard to get one’s bearings these days.
I’m afraid that my generation made it harder for you than it used to be – or needs to be…
Dr. Carroll, I was reminded of your comment about keeping things going when I read NIH turns to crowdsourcing to repurpose drugs.
If I thought science was driving this, I might not be so concerned with the implications of an approach that seems intent on searching for a disease for a drug instead of the other way around.
Mickey,
FWIW, many people with diabetes have gotten progressively worse following the ADA guidelines to eat around 50 to 60% carbohydrates. It was only when they resorted to a paleo type diet, that they greatly improved. Fortunately, many medical professionals are getting the word but many are still in the dark ages.
As one who hasn’t been diagnosed with diabetes but who definitely has metabolic issues, it is quite obvious from my glucometer readings that I need to stick to a low carb diet which I am struggling with for other reasons.
I guess my point after all of this is following checklists that are allegedly evidenced based can greatly worsen your health.
Thanks Wiley! This makes me very nervous, because baclofen seems to be getting re-purposed all over the place lately … mainly as a treatment for alcohol and drug addiction. (The other treatment they’re pushing for that — Neurontin and other anti-convulsants — have similar problems.)
Any chance you’d be willing to write up your baclofen-etc. story for RxISK? I think you basically have it written — might just need a bit more background about yourself & your experiences. You can get ahold of me at
jojoryan56@yahoo.com
John Rush retired from NUS in May. His “scientific achievements” included ‘authoring some 600 papers in high-impact journals’.
http://www.nus.edu.sg/uawards/2014/winners/augustus-john-rush.html
Click on Videos to see the awards ceremony.