This Age of Meta-Analyses in matters of the psyche is poking holes in some broadly held paradigms, nowhere more apparent than those relating to the notion of the monolithic Major Depressive Disorder. The efficacy and safety of the SSRIs are being widely re-considered. The DSM-5 Field Trials made an assault on the bedrock reliability that vaulted Major Depressive Disorder into being in the first place:
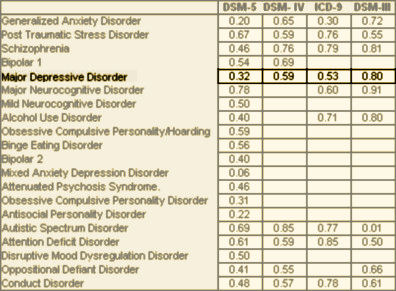
[kappa values in the DSM Field Trials]
by Tom J. Johnsen and Oddgeir FriborgPsychological Bulletin. 2015 May 11. [Epub ahead of print]A meta-analysis examining temporal changes [time trends] in the effects of cognitive behavioral therapy [CBT] as a treatment for unipolar depression was conducted. A comprehensive search of psychotherapy trials yielded 70 eligible studies from 1977 to 2014. Effect sizes [ES] were quantified as Hedge’s g based on the Beck Depression Inventory [BDI] and the Hamilton Rating Scale for Depression [HRSD]. Rates of remission were also registered. The publication year of each study was examined as a linear metaregression predictor of ES, and as part of a 2-way interaction with other moderators [Year x Moderator]. The average ES of the BDI was 1.58 [95% CI 1.43, 1.74], and 1.69 for the HRSD [95% CI 1.48, 1.89]. Subgroup analyses revealed that women profited more from therapy than did men [p < .05]. Experienced psychologists [g = 1.55] achieved better results [p < .01] than less experienced student therapists [g = 0.98]. The metaregressions examining the temporal trends indicated that the effects of CBT have declined linearly and steadily since its introduction, as measured by patients’ self-reports [the BDI, p < .001], clinicians’ ratings [the HRSD, p < .01] and rates of remission [p < .01]. Subgroup analyses confirmed that the declining trend was present in both within-group [pre/post] designs [p < .01] and controlled trial designs [p = .02]. Thus, modern CBT clinical trials seemingly provided less relief from depressive symptoms as compared with the seminal trials. Potential causes and possible implications for future studies are discussed.
Rather than speculate and obsess on the why of a waning response to CBT or the why of the plummeting kappa in the DSM Field Trials [or for that matter the why of the Placebo changes described by Kirsch [first rate madness…] or the other challenges to the reported efficacy of SSRI/SNRI antidepressants], I think I’ll just add this to the already too long list of things that discredit the idea that one can be very scientific with a category that elevates dysphoric emotion to the level of a disease entity and offers simple generic solutions. Looking at the last several posts [about Collaborative Care], there’s a whole system being built around some psychiatrist reviewing cases with a Care Manager sight unseen and making pronouncements about a treatment plan that prescribes CBT and/or Drugs to treat this obviously changing and heterogeneous category called Major Depressive Disorder.
Mickey,
I don’t understand the controversy.
If you are a psychiatrist and you don’t believe that depression exists – don’t treat it.
If you don’t believe that various antidepressants (or maybe any antidepressants) work – don’t prescribe them.
If you believe that any medication is too toxic to prescribe then it is your ethical duty to not prescribe it.
I realize that it is human nature to argue and try to convince everybody else, even to the point of absurdity. I confronted a physician on this issue myself. He was trying to convince me to not prescribe an antidepressant that I had not prescribed in decades. I said to him: “Well you seem to take the position that this is all news to me, when was the last time you prescribed that drug? You tell me and then I will tell you the last time I prescribed it.”
Dead silence – he would not say a word.
I would like to know how many practitioners who take these positions on depression and medications practice what they preach. Or are we just humoring the so-called scientists who are generating papers based on research that (like all research) is predominantly false. What does one expect in a meta-analysis of false research findings?
I would not conclude that I don’t know what I am doing based on this research, but apparently some people do.
Of course I believe depression exists. Of course I prescribe antidepressants. Of course I see anti depressants work sometimes. Of course I believe every medication can be toxic, and take care to be on the lookout. My complaint is simple. Major Depressive Disorder is a broad category, dealt with as if it is a unitary condition. It’s not. It’s a symptom that was better fractionated in even the DSM-II than the ones that followed. Having a Primary Care Doctor Dx MDD and start an antidepressant as a first line of treatment is no good in my book. I’m hardly the antipsychiatrist you’re snapping at here. I’m a person that thinks the DSM is, at best, a too thick code book. We know a lot more about the various depressive syndromes than that book implies, including the fact that depression is often a symptom of life’s ills that has little to do with the brain or even some need for a symptomatic treatment. I think that my job is to figure out where the problem lies and that category doesn’t help. The controversy is that our literature is full of Major Depressive Disorder is a Brain Disease in need of medication. Sometimes that’s right…
When it comes to effect size (which effectively is what Hedge’s g denotes) then a value of 0.2 is considered small, 0.5 would be viewed as moderate, and 0.8 or more as a large effect size. The early effect sizes reported for CBT are stupefying at 2.6 to 3.6 using the BDI in the early studies of Beck and Rush, and corresponding values of 3.3 to 4.1 using the Hamilton scale in those same studies. They had nowhere to go but down!!! We will never know what bias crept in to those studies but the numbers are a strong signal that the reports may be too good to be true.
“Of course I see anti depressants work sometimes.”
I would say if anti-depressants work sometimes – why prescribe them?
I had this conversation with the primary care docs who I work with the other day. They were talking about the 40% response rate to antidepressants and one of them said: “I would kill if I could prescribe medications with a 40% response rate.”
In the real world nobody is concerned about brain diseases or even more basic organ pathologies. It frequently comes down to if the physician thinks the patient needs the medication or not. At least that is what some of my Internal Medicine colleagues have told me over the years.
the problem i have with these medications is that they induce an (currently) immeasurable, but recognizable, effect.
my main beef with antidepressants, aside from their uncertain outcomes, is that the patient feels something is ‘working’ by taking the medication. whether it is targeting the (alleged) brain areas/locations associated with depression is another story.
however one cannot dispute that even if the antidepressants do not work as they’re marketed, they still induce a sort of dependence in the patient. i attribute this dependence to the phenomenon described above.
this is sort of like the placebo effect but instead of having ‘no effect’, it just has an effect that we can’t measure accurately. such an effect is felt by the patient, and can have disastrous effects if they do not believe the drug is ineffective.
i hope you can see where i am coming from
I’d be surprised if the metadata showed anything else. If I had to guess I’d say the major reason was due to patient groups less properly screened for the noise of comorbidity, including drugs/alcohol and Axis 2 disorders. Not to belabor a point, but this is where psychometrics have an important role in research in terms of sample screening. As previously mentioned, testing drugs with say 7/9 symptoms for a greater duration instead of 5/9 would also help screen out self-limited adjustment disorders. I’m still in disbelief that PHQ-9 is commonly used as a research measurement tool.
“……..however one cannot dispute that even if the antidepressants do not work as they’re marketed, they still induce a sort of dependence in the patient. i attribute this dependence to the phenomenon described above.
this is sort of like the placebo effect but instead of having ‘no effect’, it just has an effect that we can’t measure accurately. such an effect is felt by the patient, and can have disastrous effects if they do not believe the drug is ineffective.
i hope you can see where i am coming from”
Actually I can’t.
But I can apply the same metric that I have applied before. If I were a psychiatrist with that belief system – I would NOT be a prescriber of antidepressants.
Just to expand on Dr. Carroll’s point. The usual measure of Effect Size is Cohen’s d. That’s the one with the reported ranges he mentions above. Hedge’s g is a variant corrected for a slight population bias with small samples:
The correction approximates 1 with sample sizes like those reported here so Hedges’ g and Cohen’s d are the same. Another thing about these measures of Strength of Effect – the values are heavily influenced by the variance [standard deviation] in the samples. Here, the same difference in means produces very different results depending on the variance in the compared populations:
Another possibility is that the initial enthusiasm picked up on by the subjects produced a major Hawthorne effect that didn’t sustain over the decades.
This is going to be one of those weird threads where no one agrees about anything. Which is fine, some of those are very interesting.
Wouldn’t there be lot of reasons why CBT is less effective now that have nothing to do with CBT? It seems to me that the elephant in the room here is that things are generally more depressing than they were in 1978. That would make depression harder to shake, whether it scales as a 6 or a 9.
Inflation adjusted salaries are lower, there’s less clean water and clean air, and people have trouble talking to each other without using some kind of electronic device. Hell, the clinicians are probably depressed, too. You can’t have a consultation with a colleague three doors down the hallway a without booting up some ghastly piece of software and messaging them so it can be documented properly in the EMR.
In 1976 I was a minor and I could talk to my psychiatrist about all the crazy things I thought about and even did sometimes without mum and dud or the PET team or the police finding out, which is probably one of the reasons why I didn’t wind up shooting dope or blowing my brains out like a lot of my classmates. The modality happened to be psychoanalytic, but I probably would have done reasonably well with CBT. The whole cultural frame was much more conducive to psychotherapy in general.
Yo, if I were 17 now, and had the kind of problems I’d had then, and some dork had asked me to keep an automatic thought record– how well do we think that would have worked? I probably would knock their teeth out. Adults can get very impatient with it, too, as many of you may have observed.
I’m not at all surprised that CBT worked better back in the day. Microsoft Windows hadn’t even been invented.
Yeah, yeah, I know, n=1. And there is a lot to like about the study, particularly the fact that many of the outcome measures were the same, even if some of them were updated. It has the virtue of not seeming totally nonsensical, which is getting to be more of a plus.
And I think I do have some idea what Gagan is saying. Antidepressants definitely make people feel something, though it may not be associated with any discrete, measurable event, though I do think the discontinuation symptoms or effects associated with dosage change or cessation can be quite dangerous for some people, and I don’t think it’s an Axis II thing.
And yeah, PHQ9 seems pretty useless for research, that is just… wrong. Combined with a good intake questionnaire,though, I liked it better than QIDS for assessment– now that I think of it, I also learned a lot from notes they wrote down in the margins. Another reason I prefer paper forms to electronic ones.
Of course antidepressants incur physiological (and sometimes psychological) dependency, whether they reduce whatever was called “depression” or not. They are psychoactive substances taken chronically.
As with all the psychoactive substances, they incur neurological adaptation. Whether you think this is good or bad depends on where you sit. It certainly does not make it easy to go off them.