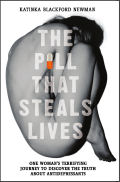
 David Healy‘s blog has a guest post called The Pill That Steals Lives: One woman’s terrifying journey to discover the truth about antidepressants by Katinka Blackford Newman – an introduction to a book about her experiences with psychiatric medications due out in early July. It’s one of those all too familiar stories where a negative reaction to one medication was interpreted as an illness that was treated by adding other medications in an escalating cycle:
David Healy‘s blog has a guest post called The Pill That Steals Lives: One woman’s terrifying journey to discover the truth about antidepressants by Katinka Blackford Newman – an introduction to a book about her experiences with psychiatric medications due out in early July. It’s one of those all too familiar stories where a negative reaction to one medication was interpreted as an illness that was treated by adding other medications in an escalating cycle:It had started when I had hit a wall of despair while going through a divorce. Sleepless nights took me to a psychiatrist who prescribed an antidepressant. Within hours I was hallucinating, believed I had attacked my children and in fact attacked myself with a knife. I ended up in a private hospital where doctors clearly thought I had a screw loose when I told them I was being filmed and that there was a suicide pact with God. The psychosis ended when I said I wanted to stop taking the escitalopram but doctors insisted I take more pills. This began a terrible decline where I couldn’t leave the house, dress myself, finish a sentence. But the worst thing of all was that I couldn’t feel love for my children, Lily and Oscar, who were 10 and 11 at the time. At the end of a year I was about to end it all. As a last resort I tried to get myself readmitted to the same private hospital, but my insurance had run out. And that was how I ended up sectioned at this NHS hospital that had made the decision to take me off all the drugs [Lithium, Olanzapine, Sertraline, Prozac, Lamotrigine]. I was climbing the walls, screaming, shouting, and begging my family to get me out of there. If I’d been suicidal while on the drugs, withdrawal made me far worse…
[Lithium, Olanzapine, Sertraline, Prozac, Lamotrigine]
[two antidepressants plus two mood stabilizers plus an atypical antipsychotic]
[glutamate with yet to be determined enzyme interaction plus a dopamine, serotonin receptor antagonist [D2, 5-HT2] plus a serotonin reuptake inhibitor [SERT] plus a glutamate voltage-gated sodium channel blocker]
The way this happens is that a patient gets started on a medication and things go badly. So other medicines are tried without stopping the last. As the patient continues to go downhill, the medications get added irrationally. There may be akathisia and/or withdrawal mixed in with the medication effects. It ends like the story I think I’ll read when the book arrives – an impossible situation where the patient still may or may not have the problem they came with, are living in an obtunded mental state from all the medications, and have the added prospect of one or more withdrawal syndromes to face. One unholy mess!
Wait. She was on all those meds AT ONCE?
Confucius say, Blame man before you blame God.
Yes, frighteningly easy to get to six or more psychotropics when symptoms are viewed in isolation, without searching for something to tie them all together. In part we can thank DSM-III and its successors for that. Also the doctor’s urge to “do something” as well as, in some cases, patient requests to add this or that (and spineless docs who comply). There’s also the discounting of harm: our meds can’t hurt patients.
Sometimes two meds are added at once when one — or none — might do. Other times the problem accrues over weeks, months, or years, as meds are added but never subtracted. While both are mistakes, the former strikes me as worse somehow.
If you find yourself in a hole, the first thing to do is stop digging.
When I teach residents I tell them that the more psychiatric medications a person is taking, the less likely that he needs them or is helped by them. Complex medication regimens which include most classes of psychiatric medications are sometimes a clue to a misdiagnosed personality disorder.
“”What the hell has happened, I wondered. I had a vague recollection of the last year, which I later called the year my life was stolen. It had started when I had hit a wall of despair while going through a divorce. Sleepless nights took me to a psychiatrist who prescribed an antidepressant.””
Can anyone please explain why since the combination of dealing with lack of sleep and and a stressful event such as a divorce likely led to depression why a sleep aid wasn’t prescribed initially like ambien? And if the treating psychiatrist still felt depression was an issue, why something like a sedating sleep aid like Trazadone wasn’t prescribed instead of an SSRI which is well known to cause sleep disturbances?
On another note, Mickey, obviously I mean no disrespect but you act shocked by all these meds combinations. Obviously, I can’t offer a pub med citation but this practice is quite common in psychiatry.
To be fair, I am trying to think if this happens in the practice of “regular” medicine and the only situation I can think of that it might occur is treating people with high blood pressure. I have heard of people on 3 medicines when it seems doctors, particularly after adding a 2nd one should be looking to see if anything unusual is going on. Of course, that is assuming the patient is doing his/her part to keep the BP down.
AA,
Re your looking for non-psychiatric parallels: even if we accept the shift away from the “mental” vs “physical” health paradigm, so psychiatric drug numbers are not compared to “non-psychiatric” drug numbers, why do you see BP drugs for an individual as the best parallel to all psychiatric drugs for that individual?
Even with the narrow view psychiatry would be dealing with the nervous system and cardiology for instance with the cardiovascular system. Between BP drugs, and statins, and anticoagulants, and anti arrhythmic drugs an even asymptomatic individual can be on a startling amount of combination therapy. Even more if you count the drugs affecting glucose metabolism given in part to try to support cardiovascular health. Infections disease cocktails are another possible example. This is not to necessarily argue that any of these situations are “good” but the tension between the terms “poly pharmacy” and “combination therapy” exists throughout medicine.
Gad Mayer:
You would think more psychiatrists would figure that out, but, we’re all ignorant of the fact that personality disorder exist as a diagnosis since managed-care ruled out as using that diagnosis for any type of reimbursement 20 years ago.
I firmly believe that medicating primary axis II disorders is contraindicated until proven otherwise. And yet, how many non psychiatrist providers as well as lazy colleague psychiatrists dump these Axis 2 patients on the doorsteps of providers like me, because they screw up the patient so much with their over-prescribing, and then expect others to bail them out!
Yes, I’m tired of this, that’s why today is my last day in private practice, and I am not looking back…
Thanks for your comment though.
Joel H, fellow colleague in arms
…and somehow, the net effect of all this is that I almost never see Axis II diagnoses on referral paperwork. So, as a newly-licensed rookie just starting private practice, I’m still not always confident when I’m seeing it and when I’m just seeing “features.”
BPD I can recognize most easily. That one seems to present very much the way it’s described in textbooks. The few BPD patients I’ve worked with seemed very attached to any medication they were taking, unfortunately, and were constantly adjusting their “cocktails.”
Schizotypal and Schizoid I have trouble diagnosing probably because of my own grandiosity– I feel like surely they won’t be that way forever if they are working with me. Neuroleptics would seem like a very odd choice for these folks, particularly the reuptake inhibitors.
Narcissistic? Honestly, I feel like I’ve never really seen this by itself, though I often see strange hybrids of cluster B that have a very strong narcissistic component and seem quite pervasive. I think it’s a real blind spot in my training, and glad this thread is making me think about it.
Also glad, Dr. H., you noted the reimbursement issue b/c as strange as it might seem, that’s not on my radar as an MFT so much– the PD patients I have seen were usually getting reimbursed under another diagnosis.
Another part of the problem, of course, is that as interns, MFTS and psych assistants and social workers are often trained not to diagnose Axis II until we’ve worked with a client for several months… and of course, in community mental health, patients are often limited to 26 sessions or less. Part of it is a reluctance to “brand” someone with an Axis II dx.
And there’s the irony– diagnoses shouldn’t be a scarlet letter that follows patients around all their lives, they should make it easier for us to understand how his previous therapist or intake or whoever was thinking about their symptoms, at least.
But I haven’t seen Axis II on a single referral since I got licensed six months ago. Not one.
I write this blog primarily because I want to fight the corrupt intrusions of commercial forces into psychiatry and our literature. But as a clinician, there are two other things that have happened since the 1980 revolution that I lament, both in the “Axis II” domain. The first is the medicalization of child psychiatry. The developmental models and the concept of developmental deviation were very useful frames even for adult psychiatrists, and most of what we hear is about drugs for “little adults.” But the other thing is Personality Disorders, particularly people with Borderline or other “Object Relations” pathology. I expect Joel’s implication is right, that many of the patients who get put on these bizarre regimens fall into that category as are many of the “bopolar” patients that don’t fit and don’t respond as expected. While these diagnoses are sometimes used in a derogatory way, that’s as wrong now as it was before 1980. These are difficult people, but their suffering is very real, and they’re in no way helped by throwing medications at them.
I know that at least 1/2 of what goes on in Community Mental Health Clinics these days is a combination of Axis 2 as primary matters along with addiction, if not even a higher percentage. Thus, it is beyond absurd what is being expected, nay, demanded of us as prescribers in “fixing” these patients who have to fix themselves.
I have never viewed or framed Axis 2 as a perjorative or biasing diagnosis, but, it is nice to know what the role of interpersonal struggles are to the presentation, and it being minimized, ignored, or plain denied especially by non psychiatrists, providers or therapist irregardless, is beyond annoying and disruptive for me.
So, I appreciate the above reply by Dr N, and just have this to say to anyone who is in the trenches I have toiled these past 20 plus years: you can’t fix personality disorders or entrenched difficulties in interpersonal skills with pills first, and other interventions later if even offered.
And, I firmly believe that primary personality problems are worsened by meds, especially antipsychotics and high dose antidepressants, and forget benzos until the last choice for any honest and tangible anxiety. But, who the hell thinks that besides me?!
Personally, I think private practice patients are eroding into more characterological/psychosocioeconomic angst that is not being problem solved responsibly or effectively by at least 50% of what I have seen this past year plus. But, if I heard one more therapist tell me to treat “Bipolar Disorder” or “PTSD out of control” once more, the growl would have become deafening, so, I am gone from that arena.
Happy Memorial Day to all.
The horror stories have become commonplace, I’m afraid — and you don’t even have to start with “psychiatric” symptoms to get sucked in. Last year RxISK ran a story from a Texas construction worker whose troubles began with back pain mis-diagnosed as Fibromyalgia. His reaction to the medication cocktail he was handed got him passed along to a shrink and diagnosed with — you guessed it — Bipolar Disorder.
Here’s the med list he ended up with: “Cymbalta, Lyrica, trazodone, Trileptal, gabapentin, Wellbutrin, tramadol, Soma, Amrix (more cyclobenzaprine), Etodolac, lisinopril and Sprix (ketorolac). Some were for physical pain, some were for bipolar disorder, and some were for both. The lisinopril was for my blood pressure.”
http://rxisk.org/my-trip-through-the-polypharmacy-blender/
My tale of woe is similar, albeit not quite so horrific – I was severely POISONED by SSRIs, could not sleep and was hospitalised and diagnosed “bipolar’ – a total joke. Such a ridiculous label…….there could be fewer people on this planet less ‘bipolar-like’ than me (when not messed up by prescribed meds). I shall never forgive the medics (foolishly influenced by Big Pharma) and am VERY annoyed that I now have a restricted driving licence. Someone should be saying SORRY to folk like me and remedying this crazy situation.
Deprescribing is often far more useful than prescribing.
Yes, it is very interesting that you hardly ever see a personality disorder diagnosis anymore when it is painfully obvious in society these are on a rapid increase especially in young people. Just look at the deterioration of campus life and some of the outrageous ways that students deal with minor conflicts and insults.
http://knowyourmeme.com/memes/trigglypuff
Not that my pathetic generation of entitled, spoiled and ungrateful boomers are a bastion of character strength.
Dr O: stop referring to this person, it’s only giving her more exposure, even if intended as negative. My brother wisely reminded me when I criticized this lame jingle on TV years ago that, “well, it might suck, but, it stays in your head and makes you think about it”.
And I do NOT want to remember this human being any more!
Anyway, Happy Memorial Day to all here, and let’s remember now when so many in leadership have no respect for the military these days, that people who die for country are the most honorable of all!
People have died so folks can bitch and moan like petty kids. Oh, I was referring to our politicians with that “petty kids” part there….
Yes, today and tomorrow are days of gratitude and never losing sight of the fact that we are all in the .001 percent of the luckiest humans who ever roamed the earth. It would be nice if the people who always complain about the 1 percent realized they are in the .001 percent. It’s not where you are in the bell curve that matters, but how you got there. Most of us are just lucky on when and where we were born.
So there’s my weekend rational-emotive rant on gratitude.
Frankly, if it were up to me, combat veterans would get permanent tax breaks and maybe extra votes.
More and more, we are starting to see the difference between citizens and civilians in public behavior. Much like Heinlein’s Starship Troopers, except that some of the least grateful civilians seem to get more privileges than the stoic heavy lifters.
I feel that if psychiatrists could experience a bout of akathisia or such like, it would change the way they prescribe, there is no way to describe to someone who hasn’t had it, what it feels like. For me, it didn’t take a cocktail of medication to do this to me. I had one injection of Flupenthixol of the lowest dose and lost 6 months of my life. I am lucky to have mostly recovered. The doctors didn’t believe me at all that I was having such a severe reaction from a single shot of the lowest dose. They said it was all in my mind and I was being non compliant. If that was the case then how come I didn’t complain about the other 11 medications I had been on in the past? But the thing is, it’s kind of normal for the average person to just assume what we say is crazy talk, literally. All my life before taking any kind of substance or medication I have always googled it first. When I came across blogs saying that psychiatric drugs are demonic and can kill you or ruin your life, I rolled my eyes. Whilst it isn’t accurate to say that any substance is “demonic” I now see just why people are describing them that way.