Articles like these are part of a great big wake-up call, and I’m not sure they’re reaching the right audience in the right ways. For the moment, I’ll just add them to the growing catalog, and pick back up next week after the national election is behind us. Right now, diversion time – World Series, Game 7!
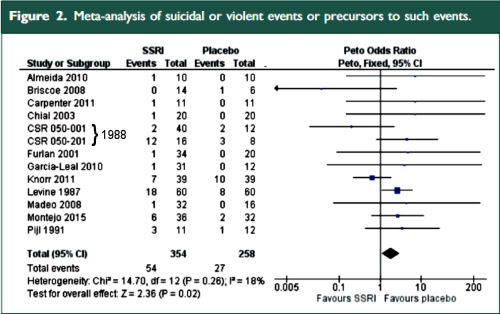
by Andreas Ø Bielefeldt, Pia B. Danborg, and Peter C. GøtzscheJournal of the Royal Society of Medicine. 2016 109[10]:381-392.Objective: To quantify the risk of suicidality and violence when selective serotonin and serotonin-norepinephrine reuptake inhibitors are given to adult healthy volunteers with no signs of a mental disorder.…Conclusions: Antidepressants double the occurrence of events in adult healthy volunteers that can lead to suicide and violence.
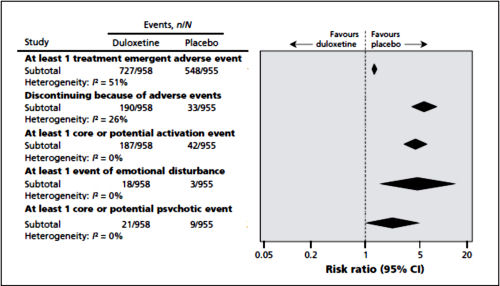
by Emma Maund, Louise Schow Guski, and Peter C. GøtzscheCanadian Medical Association Journal. First published online ahead of print on November 14, 2016.
Background: The European Medicines Agency makes clinical study reports publicly available and publishes reasons for not approving applications for marketing authorization. Duloxetine has been approved in Europe for the treatment of stress urinary incontinence in women. The reported adverse effects of duloxetine include mental health problems and suicidality. We obtained clinical study reports from the European Medicines Agency concerning use of this drug for stress urinary incontinence.Methods: We performed a meta-analysis of 4 randomized placebo-controlled trials of duloxetine [involving a total of 1913 patients] submitted to the European Medicines Agency for marketing approval for the indication of stress urinary incontinence in women. We used data from the clinical study reports [totalling 6870 pages and including individual patient data] to assess benefits [including frequency of incontinence and changes in quality-of-life scores, such as Patient Global Impression of Improvement rating] and harms {both general harms, including discontinuation because of adverse events, and harms related to suicidality, violent behaviour and their potential precursors, such as akathisia and activation [stimulating effects such as insomnia, anxiety and agitation]}.Results: Duloxetine was significantly better than placebo in terms of percentage change in weekly incontinence episodes [mean difference -13.56%, 95% confidence interval [CI] -21.59% to -5.53%] and change in Incontinence Quality of Life total score [mean difference 3.24, 95% CI 2.00 to 4.48]. However, the effect sizes were small, and a sensitivity analysis [with removal of one trial] showed that the number needed to treat for a Patient Global Impression of Improvement rating of "much better or very much better" was 8 [95% CI 6 to 13]. The numbers needed to harm were 7 [95% CI 6 to 8] for discontinuing because of an adverse event and 7 [95% CI 6 to 9] for experiencing an activation event. No suicidality, violence or akathisia events were noted.Interpretation: Although duloxetine is effective for stress urinary incontinence in women, the rates of associated harm were high when individual patient data were analyzed, and the harms outweighed the benefits.
[truncated from the original]
 The two papers combined report seventeen blinded clinical trials [scattered over 28 years] with some ~1300 non-depressed subjects on SSRI/SNRI drugs compared with ~1200 placebo controls. The findings of an increased signal for suicidality with these drugs have been traditionally discounted by critics with various rationales because the medications are being given to depressed people [who are suicide-prone anyway]. So here’s a large cohort of studied patients where that explanation obviously won’t fly. And in each case, the forest plots still show that the target adverse events are significantly more prevalent in the drug treatment group than in the placebo controls. The question then becomes, "What were those target Adverse Events?"
The two papers combined report seventeen blinded clinical trials [scattered over 28 years] with some ~1300 non-depressed subjects on SSRI/SNRI drugs compared with ~1200 placebo controls. The findings of an increased signal for suicidality with these drugs have been traditionally discounted by critics with various rationales because the medications are being given to depressed people [who are suicide-prone anyway]. So here’s a large cohort of studied patients where that explanation obviously won’t fly. And in each case, the forest plots still show that the target adverse events are significantly more prevalent in the drug treatment group than in the placebo controls. The question then becomes, "What were those target Adverse Events?"And what of the numerous and compelling case histories of suicide, homicide, violence, agitation in some people taking SSRIs/SNRIs? They are often discounted as "anecdotes" – lacking the statistical/mathematical certifcation that comes from clinical trials. They are infrequent and just don’t show up with strong signals in RCTs or population studies. So these meta-analyses are attempts at quantifying the phenomena. But again, the question becomes, "What were those target Adverse Events?" "What do they mean by precursors to suicidality?"
Here are the criteria they used in searching through the articles/reports in these meta-analyses:
[Bielefeldt et al]
[Maund et al]
In the Bielfield et al [healthy volunteers] paper, they report on "suicidal or violent events or precursors to such events" without breaking them down. And in Maund et al [duloxetine in stress incontinence] they do break them down [above]. In this latter study they mention that there were no suicidal or violent events reported in these trials [it’s worth taking a look at this paper for the suicidal info that wasn’t reported].
There was a time when I might have read these papers that talk about "suicidal or violent events or precursors to such events" yet report no actual suicidal or violent events and been mighty skeptical. But that’s not true any more – at least for me. In fact, in our recent second Paxil Study 329 paper [Study 329 continuation phase: Safety and efficacy of paroxetine and imipramine in extended treatment of adolescent major depression], we used similar criteria. Here’s a chart I made along the way that didn’t make it into the published paper [my made-up word ‘AGITA‘ being roughly similar to the "Activation" categories above]:
by David HealyPrimary Care Psychiatry. 2000 6:25-28.
In the course of a randomised double-blind crossover study comparing the effects of reboxetine and sertraline in a group of healthy volunteers, two volunteers became suicidal on sertraline. This paper describes the characteristics of the reactions experienced by both subjects. These problems were associated with a combination of akathisia and disinhihition. Dysphoric or akathisic responses on their own to either drug did not lead to suicidality in this group of subjects.
"In one of the two crossover trials we excluded because we did not have data on the first period separately, a healthy volunteer committed suicide, which was mentioned in both published articles. She had received duloxetine in increasing doses for 16 days, tapered off the maximum dose of 400 mg daily very quickly [in just four days according to the design of the study] and killed herself four days later while on placebo. The authors, several of whom were employees of Eli Lilly or owned stock in the company, judged her suicide lto be unrelated to study drug treatment, although it is well known that the suicide risk is high when an antidepressant is stopped abruptly…
In 1990, Teicher and colleagues reported on the emergence of suicidality on fluoxetine in a group of six patients. These reports were followed-up by reports from King et al., Creaney et al. , Rothschild and Locke and Wirshing et al., among others, reporting other cases where suicidality appeared to emerge in individuals taking fluoxetine.from Healy2000
To me the most critical question a psychiatrist prescribing SSRIs to adolescents faces around this is the question of whether the increased risk of death (if there is one, and would be great to this expressed more often as natural frequencies) is significantly mitigated by awareness and vigilance on the part of the youth, their family, and the treatment team.
I consider the black box warning of utility in that I believe it increases that awareness and vigilance. Even though I remain uncertain as to what I believe the overall increased risk of death to be, I have seen clinical examples that to me warrant the warning (in terms of both increases morbidity and possibly mortality). Within that context, I still see SSRIs having a role in pediatric anxiety (based on clinical experience of myself and others and clinical trials) and pediatric depression (based on clinical experience of myself and others). So given that vigilance and collaborative treatment with youth and family for the n of 1 patient in front of me, and the n of 1 monitoring of clinical impact with that patient, the amalgam of clinical trials and population level findings are not necessarily as pressing
However, there is the view (explicitly advanced by Dr. Gotzsche) that vigilance is irrelevant to the risk incurred. That the nature of the emergence of the danger(s) do not lend themselves to mitigation except by never prescribing the medication to a child in the first place. To me that question is one of the most directly relevant to the decision making with an individual youth and family.
1bym,
I obviously agree with you. I don’t see adolescents any more [because I was pressured to medicate them more than I felt comfortable doing]. And while I haven’t had that much luck in depressed kids, I wouldn’t argue otherwise. I wouldn’t look to Gotzsche et al for guidelines, but rather meta-analysis. He reports a signal for what I call Agita and I buy that result [see the next post]. Vigilance and Mitigation are in the hands of the clinician…
Vigilance being irrelevant is a statement that can be casually made by anyone not practicing psychiatry. Vigilance for all kinds of things is part of what makes good psychiatrists.
I think it is quite easy to dredge thorough clinical trials data and make whatever argument you want. In fact, I find it surprising that explicit hypotheses and outcome variable are supposed to be formulated by the people doing the heavy lifting with the clinical trial in the first place and people can come along decades later and look at boxes of old records and put together whatever story they want.
The entire reason that clinical psychiatry is successful is that it is not a clinical trial by a long shot. No psychiatrist is going to keep anyone on a drug because they are incentivized to enlist “enough” patients. No psychiatrist is going to insist that a patient take an SSRI or an antidepressant for that matter when they have done an assessment and knows that the patient does not tolerate antidepressants. The entire reason that clinical psychiatry is successful is because psychiatrists know what they are doing,
Without belaboring the point – who in the hell is going to treat a patient with 400 mg of duloxetine much less stop it in 4 days. And who cares if akathisia causes suicide? If you know what you are doing the goal is to prevent, recognize, and treat akathisia as soon as possible. Again – clinical practice is not a clinical trial and all of us have the threshold for patient injury set lower than any other physicians. We don’t get a pass because patients are supposed to die of psychiatrist illness.
All of the dire warnings implicitly to psychiatrists are an insult to a field that successfully prescribes two of the most toxic medications out there – lithium and clozapine.
If you want to blame Big Pharma for inadequately designs trials that is one thing. If you want to use studies to smear psychiatrists or suggest psychiatrists are incompetent or dangerous that is quite another. And as far as I am concerned if you don’t practice psychiatry – don’t preach to somebody who does. And as far as I know – journalists don’t practice psychiatry.
All of the dire warnings implicitly to psychiatrists are an insult to a field that successfully prescribes two of the most toxic medications out there – lithium and clozapine.
Except that about 30% of patients on clozapine go on to develop diabetes. Clozapine’s toxicity isn’t just the immediate kind. In no way am I suggesting that people shouldn’t use clozapine, because it can be a life-saving drug. But I do think that psychiatrists should be actively managing the diabetes risk.
Mostly, I agree with what you’re saying, GD.
EastCoaster,
You might be interested in this blog entry on the lowcarb RN site about why a high fat, low carb diet should be the first approach to diabetes treatment.
https://lowcarbrn.wordpress.com/diabetes/low-carb-for-diabetes/
Even type 1 diabetics, who can’t completely eliminate medication, have mostly found that by following this type of diet that their need for medication is considerably less. And many type two diabetics found that their need for medication was completely eliminated.
Hopefully, this won’t be an issue in your practice but in case it is, I think you would find this site very helpful.
EastCoaster,
You might be interested in this blog entry on the lowcarb RN site about why a high fat, low carb diet should be the first approach to diabetes treatment.
https://lowcarbrn.wordpress.com/diabetes/low-carb-for-diabetes/
Even type 1 diabetics, who can’t completely eliminate medication, have mostly found that by following this type of diet that their need for medication is considerably less. And many type two diabetics found that their need for medication was completely eliminated.
Hopefully, this won’t be an issue in your practice but in case it is, I think you would find this site very helpful.
I would be careful in the language used to describe things here. The fact is that no drug can actually *cause* a person to do anything. The last thing we want is to reach a state where people will get away with murder by saying “the drugs made me do it!”.
That said, the drugs certainly induce *something*, and as it appears that something may sometimes be anger.
As someone who has been using antidepressants for 15 years until quitting recently, I can say that I feel a lot less anger now.
I would also draw a parallel here with addiction. I had some pretty big problems with overindulging in alcohol and some recreational drugs when I was younger, but I will never accept the demoralizing idea that these things “made me” do it as if I’m not a free human being making my own choices (no matter how unhealthy).
Not sure how relevant this is, but I think we should be careful in how we formulate things.