hat tip to James O… 
by Moore TJ and Mattison DR
JAMA Intern Medicine. Dec 12, 2016. [Epub ahead of print]
That report they summarized is a bear, but they’ve pared it down into two tables that are manageable. First, how widespread is the use of prescribed psychiatric medication [expressed as % of the population]?
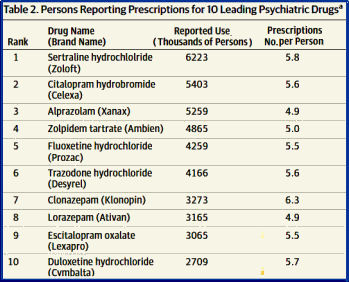
Next, which drugs are being used?
If you work in a public clinic like I do, none of that will come as any great shock. The only thing that surprised me was that
Zoloft® and
Ambien® are so high up on the list. I prescribe neither so it was just a surprise. Reasons? I had no success with
Zoloft® at all, and later, when I looked at the FDA approval documents, they looked beyond shaky to me [
zoloft: the approval I…,
zoloft: the approval II…,
zoloft: the approval III…,
zoloft: beyond the approval I…,
zoloft: beyond the approval II…,
zoloft: the epilogue…].
Ambien®? When the second patient showed up with bruises from falls while sleepwalking on
Ambien®, it came off of my formulary for good. But otherwise, no big surprises. However, the authors went further and took a reasonable stab at quantifying something that I’ve thought about [and struggled with] ever since I started at the clinic about 8 or 9 years ago –
long term use of these medications. Here are a few quotes from their letter:
"Long-term use was defined as 3 or more prescriptions filled in 2013 or a prescription started in 2011 or earlier…"
"Most psychiatric drug use reported by adults was long term, with 84.3% [95% Cl, 82.9%-85.7%] having filled 3 or more prescriptions in 2013 or indicating that they had started taking the drug during 2011 or earlier. Differences in long-term use among the 3 drug classes were small. The long-term users filled a mean [SE] of 9.8 [0.19] prescriptions for psychiatric drugs during 2013…"
"These data show 1 of 6 US adults reported taking psychiatric drugs at least once during 2013, but with 2- to 3-fold differences by race/ethnicity, age, and sex. Moreover, use may have been underestimated because prescriptions were self-reported, and our estimates of long-term use were limited to a single survey year…"
"Among adults reporting taking psychiatric drugs, more than 8 of 10 reported long-term use…"
Having taken something of a 25 year long sabbatical from mainstream psychiatry after leaving academia for a private psychotherapy practice, I started volunteering in local charity clinic after I retired. I was unprepared for the psychiatry I encountered there. I expected that I’d have to bone up on my psychpharmacology [and I did], but I sure didn’t care for what I found. It seemed like over·medication, poly·pharmacy, inappropriate drug choices, continual use of time·limited medicines, all were standard operating procedures. So I started reading the clinical trials and learned about ClinicalTrials.gov, Drugs@FDA, PubMed, and the push·back – the blogs and literature that were developing around these topics [and I started this one of my own].
This report by Moore and Mattison well documents what I found returning to general psychiatry. I still find the figures staggering, but the one that makes the least sense is that these medications are being taken long term. Depression, even in its mest malignant format is time limited for the most part. There’s evidence that in some depressions, maintenance medication can be a relapse preventive, but hardly in 80% of the cases. All of this has happened in a period where psychiatry has been telling itself and the rest of the world that it’s medicalizing, but there’s nothing about those figures that’s medical. It’s contaminated by profiteering, plain and simple, and at the expense of patients who’ve come for help.
I hear from patients who are caught up in a carousel of medications trying unsuccessfully to find something that helps but getting nowhere or even seeing their symptoms worsening:
There was a time that the best advice would be to forget what they’ve been told to date and start over, tapering any medication that isn’t clearly helping. Check out the hardware [a medical condition or medication that might be contributing]; likewise with the firmware [a major psychiatric syndrome like Melancholia or Manic Depressive Illness]; and then the software [find a reputable therapist to help them explore their lives, past and present, looking for the tangles]. That’s the same advice they would have gotten forty years ago. And it’s still good advice.
This coin has another side. While the figures quoted in this article telegraph the clear message that these medications have been over·promoted and over·prescribed, they also raise another potential concern. When we became disappointed with mental hospitals, we shut them down rather that right-size them. When we were disillusioned with antipsychotic medication and community care, we did the same thing [and filled our jails]. Similarly, when the various psychotherapies didn’t live up to their early promises, they were vilified. And while we currently remain in a situation where the medications on that list are over·prescribed, that’s not to say that there aren’t a significant number of patients who are genuinely benefiting from taking them. Something about the:
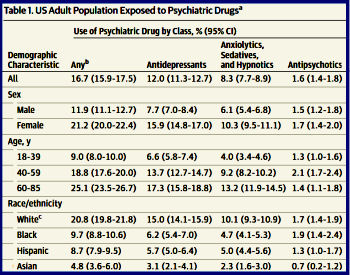
The figures don’t look that bad to me – certainly nothing that merits Szaszian rhetoric. The numbers seem roughly between the annual and lifetime prevalence numbers. Antipsychotic use actually looks shockingly low considering all of the quetiapine I have seen prescribed for sleep and anxiety. It seems that I personally have taken at least 1% of the population off of antipsychotics when they did not need them. I am guessing that written, informed consent would remove at least half of those folks.
The main problem group that I see is benzodiazepines and sedative hypnotics. Too many people taking them who are addicted to alcohol and drugs as well as the fact that there is tolerance and dose escalation particularly in the population at risk. An interesting point is that in some states the rate of opioid prescribing is twice as high as the rate of stimulant and benzodiazepine prescribing and the top decile of prescribers accounts for 60% of the prescriptions. Alprazolam 2 mg bars have high street value and active diversion probably fuels some of the list placement. The only rational approach to the problem is pharmacosurveiilance:
http://real-psychiatry.blogspot.com/2015/12/the-beginnings-of-true.html
Combined with that feedback – there also needs to be actual solutions provided to practitioners. Since practically all of the drugs on the list have been generic for some time – I doubt that drug promotion has had much of an impact. The problem at this point in time is that psychiatrists have no input into the practice models that have been foisted upon then and they come in limited varieties for employed psychiatrists. All of those varieties are based on brief visits focused on medications and forcing complex problems into that paradigm. There are no centers of excellence for treatment only centers for medication checks.
There is also a couple of issues that can’t be accounted for in clinical trials. Clinical trials are all incredibly reductive (and I am a reductionist). Doing rather exhaustive evaluations and asking people about their psychotherapy experience certainly illustrates that is no panacea and there is an incredible amount of time and money squandered on ineffective therapy. People in practice are confronted with people who are chronically anxious and depressed with no good solutions. There are many people who get partial relief from some type of medication or take it for other reasons. To me that certainly does not suggest that medications are inappropriately applied but that there is a general lack of effective treatment for a large number of people. You can certainly frame that as “if all you have is a hammer..” but to me the reality is that there is a lack of effective individual rather than population based treatment. The other issue is that clinical trials of who needs maintenance treatment are inadequate and will never be adequate. I have seen too many people who have been tapered off of antidepressants for one reason or another with very bad results. How many times do you need to be burned before you realize that maintenance medication might be required?
The other element operative here of course is that there are a group of American physicians in general are clueless about prescribing medications that reinforce their own use or addicting medications. The morbidity and mortality of the opioid epidemic is clearly the worst medication related plague that I have witnessed in my career. Any purported damage by antidepressants or antipsychotics must be trivial by comparison.
In Canada, there were 47 million prescriptions for antidepressants filled in 2014. There are only 35 million people in the country. There were 11 million prescriptions for anti-psychotics filled in the country. In one year. I consider this to be a level of prescribing that is out of control, beserk, irrational, and just plain stupid. How on earth do you defend 11 million prescriptions for antipsychotic medications in a country of 35 million people?
Eric, it’s done by a sleight of hand that we might call terminology creep, as here. If fits with RDoC, too.
“In Canada, there were 47 million prescriptions for antidepressants filled in 2014. There are only 35 million people in the country. There were 11 million prescriptions for anti-psychotics filled in the country”
If those are monthly refills plus one off scripts with no followup plus Elavil or Trazadone for sleep the numbers aren’t all that startling. What is important is the number of people on a med at one time for a specific indication as a percentage of the population. I think this is an incidence vs. prevalence error and misleading. If 4 million people in Canada are on antidepressants and 1 million on antipsychotics that wouldnt shock me at all.
I think George Dawson upstream in the comments hit the nail squarely on the head, practioners need solutions and education. I vividly remember talking to my excellent GP about the difficulties I experienced coming off longer term use of a z-drug (sedative hypnotic), zopiclone. My psychiatrist, the head of Adult Psychiatry at a major teaching hospital, dismissed my concerns and told me that I had an “underlying sleep architecture” issue that was due to bipolar and that necessitated my continued use of this medication for the rest of my life. He “round binned” the Ashton manual I had brought to him outlining a tapering schedule and I was left to my own devices to design an 8 month taper. I did receive help from the addictions medicine outpatient personnel of that same teaching hospital and I gratefully accepted that help even though I was not “addicted”, just dependent and experiencing tolerance withdrawal even while on the medication.
I accept responsibility for taking these drugs after my late husband’s suicide at the end of 2008 when I stopped sleeping due to intense bereavement and stress. I don’t blame my psychiatrist for being ignorant but I do wonder how it can be, in this day and age, that this sort of ignorance abounds within the profession.
I am happy to say that I have been off all mood stabilizers and two different antidepressants since I found a wonderful physician who helped me with bio-identical hormones and put me on the road back to wellness in 2010. I designed my own taper off the last of the medications, zopiclone, in the fall of 2012 and jumped off that drug in the spring of 2013. It has taken me over 3 years to properly heal, I still have some lingering issues due to protracted withdrawal.
Human distress in the face of real life problems and trauma is real. I keep wondering when psychiatrists are going to wake up and start practising properly, along the lines of Dr. Nardo and amazing psychiatrists like Dr. Kelly Brogan. Doctors who are speaking out about the abuses and manipulation and disinformation and just plain ignorance.
I’ve long since “undiagnosed” myself of all psychiatric labels. I’m back working fulltime again and helping others to safely withdraw from these medications with the assistance of some wonderful doctors who “get it”. These medications have their place but the widespread polypharmacy that has gone on in the name of “evidence-based medicine” since I came of age is terrifying.
Kudos to you Dr. Nardo for speaking out and continuing to hammer away at things that should be self evident to any sentient being.
Nowadays when I see the supposedly Einstein quote of doing the same thing and expecting a new result. I think exclusively on GSK’s repeated attempts at finding something positive on Paxil in adolescents or children. The drug was never safe nor effective, but still they tried atleast two(?) more times. That to me is insanity. Insanity at the cost of childrens health.