by Matthew P. Hyett, Michael J. Breakspear, Karl J. Friston, Christine C. Guo, and Gordon B. ParkerJAMA Psychiatry. 2015 72[4]:350-358.
IMPORTANCE Patients with melancholia report a distinct and intrusive dysphoric state during internally generated thought. Melancholia has long been considered to have a strong biological component, but evidence for its specific neurobiological origins is limited. The distinct neurocognitive, psychomotor, and mood disturbances observed in melancholia do, however, suggest aberrant coordination of frontal-subcortical circuitry, which may best be captured through analysis of complex brain networks.OBJECTIVE To investigate the effective connectivity between spontaneous [resting-state] brain networks in melancholia, focusing on networks underlying attention and interoception.DESIGN, SETTING, AND PARTICIPANTS We performed a cross-sectional, observational, resting-state functional magnetic resonance imaging study of 16 participants with melancholia, 16 with nonmelancholic depression, and 16 individuals serving as controls at a hospital-based research institute between August 30, 2010, and June 27, 2012.We identified 5 canonical resting-state networks [default mode, executive control, left and right frontoparietal attention, and bilateral anterior insula] and inferred spontaneous interactions among these networks using dynamic causal modeling.MAIN OUTCOMES AND MEASURES Graph theoretic measures of brain connectivity, namely, in-degree and out-degree of each network and edge connectivity, between regions composed our principal between-group contrasts.RESULTS Melancholia was characterized by a pervasive disconnection involving anterior insula and attentional networks compared with participants in the control [Mann-Whitney, 189.00; z = 2.38; P = .02] and nonmelancholic depressive [Mann-Whitney, 203.00; z = 2.93; P = .004] groups. Decreased effective connectivity between the right frontoparietal and insula networks was present in participants with melancholic depression compared with those with nonmelancholic depression [χ² = 8.13; P = .004]. Reduced effective connectivity between the insula and executive networks was found in individuals with melancholia compared with healthy controls [χ² = 8.96; P = .003].CONCLUSIONS AND RELEVANCE We observed reduced effective connectivity in resting-state functional magnetic resonance imaging between key networks involved in attention and interoception in melancholia. We propose that these abnormalities underlie the impoverished variety and affective quality of internally generated thought in this disorder.
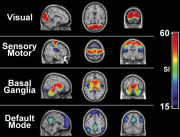 [This is a rough stab at introducing their methodology from one boring old psychoanalyst – so be gentle]. 25 years ago, Seiji Ogawa discovered that the MRI could detect the difference between oxygenated and deoxegenated hemoglobin. Since neuronal activity uses oxygen, it meant that we could actually see areas of increased neuronal activity in the brain – the blood-oxygen-level dependent contrast imaging or BOLD technique. We’ve all seen the pictures of areas in the brain lighting up in response to various stimulus. Attention then turned to the brain at rest, without stimuli [Resting state fMRI] where a number of consistent functional areas have been identified. These functional areas in the resting fMRI are connected, detected by timeline studies of simultaneous activity, so connection [and the direction of these connections] can be determined by some statistical/mathematical analyses beyond comprehension by most of the earth’s population – certainly mine. These connections [networks] may be visible [eg connectomes] or functional. Thus ends my stab at an intro to their methodology.
[This is a rough stab at introducing their methodology from one boring old psychoanalyst – so be gentle]. 25 years ago, Seiji Ogawa discovered that the MRI could detect the difference between oxygenated and deoxegenated hemoglobin. Since neuronal activity uses oxygen, it meant that we could actually see areas of increased neuronal activity in the brain – the blood-oxygen-level dependent contrast imaging or BOLD technique. We’ve all seen the pictures of areas in the brain lighting up in response to various stimulus. Attention then turned to the brain at rest, without stimuli [Resting state fMRI] where a number of consistent functional areas have been identified. These functional areas in the resting fMRI are connected, detected by timeline studies of simultaneous activity, so connection [and the direction of these connections] can be determined by some statistical/mathematical analyses beyond comprehension by most of the earth’s population – certainly mine. These connections [networks] may be visible [eg connectomes] or functional. Thus ends my stab at an intro to their methodology.  What Matthew Hyett et al did was to run resting fMRIs on 16 subjects each, from three cohorts – normals, non-melancholic depressed people, and a group with Melancholia. They identified five of the functional areas and studied their connectivity in each group. What they found was a clear separation among the three groups – documenting "reduced effective connectivity in resting-state functional magnetic resonance imaging between key networks involved in attention and interoception in melancholia."
What Matthew Hyett et al did was to run resting fMRIs on 16 subjects each, from three cohorts – normals, non-melancholic depressed people, and a group with Melancholia. They identified five of the functional areas and studied their connectivity in each group. What they found was a clear separation among the three groups – documenting "reduced effective connectivity in resting-state functional magnetic resonance imaging between key networks involved in attention and interoception in melancholia."
Despite advances in pursuing the neurobiological causes of clinical depressive conditions, the literature is characterized by divergent findings, likely reflecting their heterogeneity and varying causes. One such condition, melancholia [previously termed endogenous depression], has long held consistent ascriptions: being genetically weighted, having prominent biological perturbations, evidencing overrepresented clinical features, and showing a greater response to physical therapies than to psychotherapy. As psychiatry strives toward a diagnostic nosology based on genetic, behavioral, and neurobiological criteria, melancholia arguably represents a canonical test case…
Historical failure to identify specific neurobiological correlates of melancholia is consistent with recent advances in cognitive neuroscience that regard the brain as a complex network, whereby psychiatric conditions reflect changes in functional integration rather than perturbations within an isolated region. Large-scale brain networks supporting mood regulation, interoception, and cognition [eg, concentration and attention] are thus likely candidates for furthering understanding of melancholia’s neurobiology…
Conclusions: We position the neurobiological features of the spontaneous dysphoria of melancholia as a weakening of interactions among regions that subserve attention,mood regulation, and interoception. Computational accounts of internally generated thought highlight the importance of a critical homeostatic balance between stable self-regulation and dynamic instability. We propose that our findings reflect a loss of this optimal balance, undermining the adaptive role of interoception.
This work moves the ball down the field. As Dr. Mickey suggests, it also illustrates how a focus on a well-defined type of clinical depression can get us further than just signing up all comers with nominal, generic “major depression.” The authors spelled out a number of needed future studies that could flesh out these initial findings. It would be nice as well if they could proceed from describing statistically significant group differences to conducting conditional probability analyses of explicit criteria for group membership.
So – certain patterns of thought, feelings and other more overt behavior are accompanied by certain patterns of fMRI identified brain activity. Does this mean the brain activity CAUSES the behavioral patterns… or might it be the other way around? Where does this allow us to intervene? Not to speak of the issues of “INFERRED spontaneous interactions among these networks using dynamic causal modeling.” As BF Skinner puts it: “The effects of deprivation and satiation on behavior are not the same as the events seen through a gastric fistula… Both sets of facts, and their appropriate concepts, are important -but they are equally important, not dependent one upon the other. Under the influence of a contrary philosophy of explanation, which insists upon the reductive priority of the inner event, many brilliant men who began with an interest in behavior, and might have advanced our knowledge of that field in many ways, have turned instead to the study of physiology. We cannot dispute the importance of their contributions, we can only imagine with regret what they might have done instead” (Skinner, 1961/1972, pp.325-326). Skinner, B. F. (1972). The flight from the laboratory. As reprinted in Cumulative record: A selection of papers, 3rd edition. New York: Appleton-Century-Crofts. (Original work published 1961)
Mechanistic accounts, computer metaphors have not brought progress. I regret how very many good minds are wasted as the failure of clarity of strategy of science continues to lead to unhelpful, reductionistic accounts.
Sorry for ongoing comments (one more to come) but a paper succinctly detailing the philosophy of science problems with this study is here http://www.ijpsy.com/volumen1/num2/23/some-notes-on-theoretical-constructs-types-EN.pdf
Regarding Gordon Parker – worth noting DISCLOSURES FROM BLACK DOG ANNUAL REPORT 2010: Professor Gordon PARKER – Member of National Advisory Boards for Lundbeck. Advisor to Servier Pharmaceuticals. Speaker for meetings sponsored by Eli Lilly, AstraZeneca, Lundbeck, GlaxoSmithKline, Pfizer and Servier.
And re Parker’s solid science – his latest papers on “diagnosing bipolar 2” and then “treating bipolar 2” in Australasian Psychiatry illuminate how psychiatry has become a pseudoscience at the top levels. The first notes “My personal views which infiltrate, if not infect, this article can be summarized – and with the hope that they are contagious. As most have been detailed and referenced extensively in earlier monographs,3,4 this article will mainly weight nuances assisting diagnostic judgement.” – there is not a SINGLE scientific analysis of the 16 questions the august Prof Parker suggests we use. Contrast this with real behavioral science – “the Acceptance and Action Questionnaire (AAQ-II) assesses the construct referred to as, variously, acceptance, experiential avoidance and psychological inflexibility. Results from 2,816 participants across six samples indicate the satisfactory structure, reliability, and validity of this measure. For example, the mean alpha coefficient is .84 (.78 – .88), and the 3- and 12-month test-retest reliability is .81 and .79, respectively. Results indicate that AAQ-II scores concurrently, longitudinally, and incrementally predict a range of outcomes, from mental health to work absence rates,that are consistent with its underlying theory. The AAQ-II also demonstrates appropriate discriminant validity.” – that is SCIENCE and not opinion.
Then on treatment: “Thus, the management nuances proposed here are similarly personal – principally because of the lack of a substantive evidence base – but allowing a template for consideration by clinicians. … I personally view lamotrigine as distinctively superior to all other mood stabilizers … It is not uncommon for a medication to show quite contrasting levels of benefit in its evaluative randomized control trials and in ‘real world’ clinical practice. … (and sans substantive empirical data)… I judge lamotrigine as distinctly beneficial for some 60% of bipolar II patients and with a cost:benefit profile superior to all other candidate mood stabilizers. (Disclosure The author has been funded by a generic manufacturer of lamotrigine to provide several educational presentations over the last 2 years, and has been funded by manufacturers of other psychotropic drugs to lecture on bipolar disorders for an extended period.) On Managing acute depressive episodes
I judge such guideline recommendations as generally unhelpful and impractical. … Thus, my approach is to immediately prescribe an antidepressant with a mood stabilizer (rather than delay initiation of the former) after warning the patient about risks, reviewing at frequent intervals and, if required, also adding augmenting medications (such as a low-dose atypical antipsychotic for a brief period). Once the patient is out of the episode, I attempt to first cease any antipsychotic and subsequently the antidepressant. Approximately one-third of patients presenting with a severe bipolar depression appear to subsequently manage on a mood stabilizer alone, one-third need an antidepressant as an ongoing or intermittent strategy, and the remainder need several medication classes in combination.
– all this without any empirical support, personal clinical impressions, and with the self-annointed BP2 Dx, the self-judged BP2 Rx, 1/3 will be on 3 drugs as maintenance from first “BP2 depressive” episode onwards.
I’m afraid this is far from “solid science”. See Australasian Psychiatry April 2015 for both articles (highly influential on Australian psychiatric practice, entirely anecdotal, and simply opinion pieces) in full.
hahahahahaha psychologist