At the beginning of the week, I worked in the clinic. One of the patients I saw was a woman in her early thirties with increasing depression over the last year. She’d been seen several weeks earlier by a Nurse Practitioner and started on Citalopram which had helped "some." Her story: In spite of being a good student, she had quit school as soon as she turned sixteen and married. By her mid-twenties, she had four children [now ages 9 through 16]. The part of her history that caught my attention was that she also had "two babies" age 1½ and 2½. Doing the math, 9-2½=6½. So she’d started this second family when her youngest had entered school. Exploring the why? of that, I hit pay dirt.
She and her sister had been raised by parents who were little more than children themselves, lifelong substance abusers who provided the amenities, but did little parenting ["we ran wild" "we raised ourselves"]. Her mother was given to "going off" for varying periods of time. The net result from this un-parented childhood was a lifelong intense fear of abandonment that literally organized her experience. Her husband had "rescued" her from her "crazy family." Then her children became her life, and she had to struggle not to be overprotective. She had a crisis when her youngest went to school, and actively chose to fill her "empty nest," but then realized that she felt "trapped" by six children and having no life outside of her family. Her oldest, a sixteen year old daughter had gotten her "first boyfriend," and for my patient, that was a double-edged sword. On the one hand, it meant that her daughter was going to leave [at some future point], tapping into her preoccupation with abandonment. On the other hand, it confronted her with how she had prematurely ended her own childhood when her own "first boyfriend" came along.
There was a lot more to this story, but that’s enough to get at what I’ve been thinking about ever since. She reminded me of lots of patients I saw when I was an Internist, cases where I knew there was something that needed to be understood, but I didn’t know how to figure out what it was. Back then, I doubt I wouldn’t have ever gotten to her fears of abandonment, much less seen how her childhood related to this adult depression. But nowadays, I doubt I could miss it. But that’s because an army of teachers, supervisors, case conferences, book authors, patients, etc. taught me how to conduct an interview, how to always have a life timeline running, how and where to listen, what kind of things can happen in a childhood, what being a mother is about, and the million other things that automatically run in the background when I’m listening to a patient. It’s an acquired intuition, but I can’t take credit for anything other than sticking to the task of learning.
So the thing I’ve been thinking about since my last clinic day is still Collaborative Care. I’ve been thinking about why I have such a visceral negative reaction when I read about it, yet it’s something I already do every time I’m in the clinic. Almost any psychiatrist that works in a clinic does it all the time. I did it Tuesday, with the LPC, a Doctor or two, a Nurse. Hallway consults. The difference between what I already do and what I read about is that I always have the option to see the patient in my version. And when I look at the diagrams, in this one, talking to the patient doesn’t even seem like an option [it says "(medication) recommendations"]:
and in this one, they go out of their way to say "infrequent" for contact with either the primary care physician or the patient:
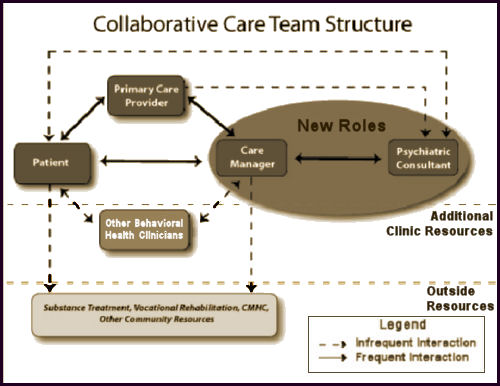
In either case, this model strips me of the only real value I bring to the table – my acquired intuition. And it implies that the first [or perhaps only] treatment for mental illness is medications. If that’s true, they don’t need a psychiatrist. They need some algorithms. Little wonder that my reaction to Collaborative Care is so negative. And little wonder so many patients are over-medicated. My guess is that the main reason for the firewall between patient and psychiatrist is some kind of cost containment maneuver.
As for the case I mentioned above. Once her abandonment fears were on the table, any number of solutions were immediately apparent. One reason she was never away from her kids was she never wanted them to feel "abandoned" – an idea easily dispelled. And there were other resources available to help her get some freedom and "have a life." She wanted to finish school and perhaps train for work outside the home. Both of those things are easy to arrange. Her husband was with her in the clinic, and hearing her fears, he came up with all kinds of ways he could [and would] help her. He seemed relieved to know how she felt.
Yes that is also what our family needed too (and finally got from the right psychiatrist) – an acquired intuition from someone who had a lot of experience of the type of extreme distress our loved one was going through. We needed someone who would listen to the details of our life,, who was willing to listen and sift through all the information we gave, someone who knew which ‘bits’ were likely salient to our loved one’s difficulties, someone who could recognize patterns that might be important and ultimately someone to help us how to understand the ‘distress’ and to understand how to ‘be’ with our loved one in a way that could facilitate positive change. It has been a slow, painful, long road but it is so far working………..
Listening, taking a developmental narrative with empathy, applying acquired clinical intuition, understanding contextual factors (past and present) surrounding symptom formation– all of this has no place in psychiatry going “forward” in this “collaborative” care matrix. This stuff takes TIME. I was in a “team” meeting at our university-based clinic and I told the residents: “Some aspects of Organized Psychiatry may rule personal history and psychodynamics out of court (and out of DSM), but I assure you that your patients will be throwing their psychodynamics in your face and you had best learn something about it or else you will be horrible psychiatrists.” My comment was met with stunned silence and then, happily, with agreement.
I’m in an epicenter of collaborative care, and have done quite a bit of this type of work, while in other parts of my job doing general psychiatry and psychotherapy with the same individual focused sensibilities that you describe. Yes, psychiatrists working anywhere around community mental health centers understand collaborative, team based care where psychiatrists share the load with others. The collaborative, primary care model in my experience works as well as the care manager. If you have a caring and experienced social worker who can approach patients with an intuitive ear and conceptualize them according to a variety of psychotherapeutic models, you’re in great shape. In actual primary care settings where I see this rolled out, it’s not uncommon for psychiatrists to also see patients up to 50% of their time. Often these consults can be cool because the care manager has gathered a bunch of longitudinal observation and collateral reports for you both to put together. Seeing patients occasionally together can allow the psychiatrist and care manager to understand how the other works. Very rewarding stuff. Unfortunately, I share your fears that in less thoughtful and barer bones roll outs of this model, psychiatrists can be be left with a rather thin, medication and biomedical focused role. As one of the other commentators so astutely observed, actual working clinical psychiatrists need to be seeing patients and understanding how individual narrative and psychotherapeutic factors are inherent in each patient encounter. I suspect that even before collaborative care, there has always been an easier ways out of just measuring symptoms and giving meds or, earlier, just reducing everyone into a few cliched psychodynamic metaphors. You older guys with your robust psychodynamic training hopefully will keep stickimg around as long as possible!
I think the difference is not simply that in the clinic you always have the option of seeing the patient, while in the collaborative care model, you, as the psychiatrist, will rarely see a patient. I think it’s that only someone with your knowledge, training, and experience will pick up on when there’s more to the story that needs to be addressed and bring that information into the picture as a way to determine how to help the patient. If the only tools available are a PHQ-9, a medication algorithm, and a care manager who has been given a two day training session prior to starting the work (I’m not exaggerating. This is in the description of how the training was done for the University of Washington model, although I’m sure some care managers have more experience), then a whole lot is going to be missed, patients will be overly or unnecessarily medicated, and not many people will be helped.
I’m not surprised academics support the model since they won’t have to deal with the negative consequences. What is astounding is the childish naive behavior of the rank and file supporting the organization that supports the destruction of their practice. Turkeys voting for Thanksgiving. The APA tries to reassure about the malpractice risks, but there is no way this doesn’t increase with a bigger patient load and the absence of a direct examination:
https://www.psychprogram.com/news/Integrated-Care-booklet_6-2014.pdf
To the psychiatrists out there who like this model, if this is such a great idea why do cardiologists do their own exams?
Um, I have been doing Locum work on and off for the past 5 years, most of it for out patient clinics, and maybe it is the premise of being a temp doc, but, these clinics by in large aren’t interested in a biopsychosocial model anymore.
Nope, they are about doing the minimal work for therapy and social needs, and just getting the patients into the psychiatrist’s office to be on meds, and then providing therapy on a monthly basis. Really, these therapists I have had the misfortune of working with think that seeing patients q month is the standard of care. Yeah, all those Axis 4 issues, really going to improve with psychopharmacology. Oh, and these therapists, they now think they can direct what meds are to be prescribed as well.
So, maybe I have been living in the Twilight Zone as an unfortunate psychiatrist, but, I really think this is the standard of care for most CMHCs of late. Maybe Dr Nardo is in the exception of the process, but, I would hazard to guess his infrequent visitations are either treated as royalty, and staff will suspend their usual behaviors for his wisdom, or, he might be a tad oblivious to what goes on those other 4 days of the week.
That is not a swipe at you, Dr N, but, I would ask you to consider walking in unannounced one day and observe what goes on in your clinic you provide care for and see what is really happening. If I am wrong, you and the rest of the system are happy. If I am right, well, you are being swindled, but moreso, so are your patients.
Terminal optimism, or complicit realism. That is my pick for most who are trying to make a difference for the Community Mental Health care population.
Hey, I have been doing the work, I have the right to voice this perspective!
Joel,
It’s not a Community Center. It’s a volunteer clinic started by some retired docs who lived in a retirement community in this otherwise rural place. The staff is all volunteer retired people from several retirement communities and we see only poverty patients. They raise the money with golf tournaments and donations. I am the only mental health type in the mix of doctors. There are two LPCs who come and do counseling. I’m not surprised at what you’re saying here. You couldn’t have known what kind of clinic it is because it’s the only one like it I’ve ever seen. We have a retired Dean of a Medical School working in our little pharmacy, and former bank presidents as escorts. I don’t live in the retirement community, but they’ll take anyone willing to come work. It’s called “good sam” [as in Good Samaratan]…
I find this whole discussion heartwarming. (and scary). I’ve been in a discussion this evening on my tumblr with two med students who are choosing to go into psychiatry. They really sound like they want to be the kind of psychiatrist that Mickey is, and I hope I am. They see the problems they will have to confront and they are going into psychiatry anyway. I have some hope that they, as they become “used docs,” with a few dings and scratches, will find ways to take the time it takes to do the work well. The discussion here shows that some of us are still holding out for that.
It is important to remember that the ACA has resulted in the closing of a number of charity clinics. Hospitals are now signing up patients without insurance and putting them in their system. This same care for all does have some flaws.
The charity clinic serving a geographic area will be sensitive to the problems of their patient population. Low incomes, access to proper diet, meaningful employment and the list goes on.
The hospital system may only be interested in generating income. This will result in additional testing, time from work and child care issues, and in the case of one local hospital the closing of all inpatient beds. There was an article at the same time breaking down the profit of a hospital based, med check only practice, and the numbers were astronomical.
Not that long ago one local high school had a graduation rate of less then 50%. Thankfully that has changed and now the rate is over 80%. There is a bubble of people who not doing well in school, and with the mills closing, found having children provided an income. Their job became knowing and using the welfare system.
Today there is a drive for additional education and training and thankfully the teenage pregnancy rate has declined. The local community college has not stopped expanding and most importantly the attitude of young people has changed.
Back to the bubble. This group represents a large part of the troubled population with a high incidence of drug addiction, crime, and gang activity. Mom and Dad told them the mills would be back and it was a company’s responsibility to give them a job.
Simply running these people through a system with a nice building along with their middle class counterparts, giving them a drug they may or not be able to afford or will choose to sell, does not solve their problem.
Understanding your patient population is key to health. A pedi I know started in a charity clinic and cannot wait to retire so as to return. The push of having two practice managers who over book and a limited hospital approved formulary has made practicing medicine impossible.
Mickey is practicing real medicine where I am sure the other doctors all play to his and their strengths. Mickey will see patients with mental health issues while the other doctors see patients that reflect more of what they did in a past life.
When a patient is a number, not a name, and meds are the answer, bad things will happen.
Steve Lucas
Gene,
I’ve made the case in another thread that if they are seeking that kind of education perhaps the better route is flex internship then Ph.D.
Fortunately my residency was balanced between psychodynamics and biological psychiatry. By today’s standards, it would be considered too psychodynamic.
But here’s the thing…in 1985 I was treating people with 200 mg Elavil, antipsychotics like Haldol, and the now defunct non-tricyclic Merital. Drugs that are almost never used today (except for headaches and sleep), and one that was withdrawn. By 1990, psychopharm had completely changed. Psychodynamic psychotherapy, like anatomy, really hasn’t changed that much.
What actually happens in psychiatric education is that the drug therapies you learn change and you really learn to keep up through reading and CME. I didn’t learn SSRIs or Lamictal or SGAs in residency because they didn’t exist or were considered too risky (Clozaril). The one thing that residency should teach is the core of psychodynamics that really doesn’t change. For example, concepts like the hierarchy of defense mechanisms remain useful for one’s entire career. If you don’t learn that early there is little incentive to learn it later especially if you get into a medication or collabocare practice.
Unfortunately there are a lot of financial and ideological incentives now for residencies to go full bio. I think this is roughly akin to the formation of the European Union, great in theory but a disaster in practice because it ignores unpleasant truths about human nature. Ironically, if the so called thought leaders of that had fully thought through the realities of European group psychodynamics (incompatible notions of fiscal responsibility between the North and South) the EU would not exist.
really stimulating conversation here.
in alberta we had a mental hospital and i just have a hard time believing anyone who did psychiatry early on (the 80s and earlier) would consider these new residents to be psychiatrists in any form.
we need mental hospitals and any real psychiatry resident, if he truly wants to ‘help’, should understand that the patients are the most unpredictable and potentially dangerous. psychiatry and neurology have been abused for decades because the powers-that-be knew they could use the media & push through drugs that didn’t show any benefit over their predecessors.
the one thing i’m most excited is what you’re alluding to dr o brien: a psychiatry education that is independent of the pharmaceutical aspect and focuses on the ‘psychodynamics’ (i call it a blend of electromagnetism and study of the psyche).
mechanisms mechanisms mechanisms
I have real concerns about the collaborative care model, but I was talking to the pharmaco-epidemiologist at work who was arguing that PCPs should be triaging the depression, because there are not enough psychiatrists. (He was from Vermont.) This is true, and I’m just not sure what to do to get around the problem.
At the fancy hospital, I’m currently working at, there are a number of primary care practices affiliated with it, some of which are community health centers. And, when it comes to primary care, population health the community health centers are more collaborative. Everyone communicates, but if somebody needs to have their blood pressure checked -even when they don’t want an appointment- or the doctor didn’t order an A1C when he should have, the nurses make it happen. At the fancier clinic, annual physicals are only 20 minutes.– fee for service volume-driven care at its best, whereas the internists at the community health centers spend more time with their patients – usually 30 minutes for a follow-up.
But I do think that there must be a model where skilled social workers spend more time with patients than the psychiatrist does and then discuss the patient in conferences. Well-trained social workers know about more than the PHQ-9.
I do think that we need cost containment in health care as a whole. Too many tests are ordered for a lot of people, too much interventional care is ordered that’s of marginal value (especially at the end of life), but psychiatry isn’t the area where we really need the cost containment.
(There is a legitimate question about how much doctors should make. Is $150K enough? They might complain, but I know engineers with good degrees from Waterloo who are making 40 or 50 with several years of experience, and those are highly skilled and educated people. But doctors always whine about this)
How are we possibly going to get enough psychiatrists to fill the unmet need? That is a serious question.
Sounds like advocacy for straight forward assembly line health care interventions, just put the patients on a conveyor belt and sent them down to be poked and prodded, and given the slip at the end for their total.
The dumbing down of medical care, really, who needs a doctor when there are so many others who can do it cheaper and faster?
Yeah, but, when the accountability comes due for the screw ups, who has the malpractice coverage? Fascinating where folks stand in the room when the excrement is headed towards the fan, eh?
East coaster-
Maybe it is because I come from Vermont and because I know how challenging it is to recruit a good psychiatrist that I find myself sympathetic to what you write. I also can think of many instances in which non-psychiatric physicians are able to offer advice in the absence of seeing the patient. While I think in our work, we should be cautious about opining without meeting the person I also remain unconvinced that a lot of what is being described here under the label of good humanitarian psychiatric care (which I endorse) can only be done by a physician.
No, Sandra, it is not just because you are from Vermont. I haven’t practied in over a year because I can’t afford to do any more volunteer work and I’m too old to work 60 hours a week in a clinic (and my potential employers know it!)
However, here in LA, what I have seen is more like the model EC describes, which is also more like the world my classmates describe– case conferences, but with plenty of client-psychiatrist contact AND rapid-fire in-the-hallway MFT-psychiatrist conferences AND scheduled sit-down multidisciplinary conferences as well.
Y’all rightly point out that “Psychiatry” is not one unified entity, and it’s absurd to talk about what “Psychiatry” thinks, etc. Community Mental Health is the same way– if anything, it’s even more riotous and balkanized. I can’t imagine how the funding streams or care delivery could ever settle into one rigid framelwork that would somehow be enforced in multiple settings. It just seems like a logistical impossibility.
God, we had one three-initial “wraparound” program at our clinic, and honestly, a lot of us never found out what the initials even stood for.
JH – do you consider it dumbing down to have systems in place to remind doctors that their diabetic patients need to be seen, that they need an A1C, and (unless the doctor makes a conscious choice not to) an LDL and micro albumin.
I really do think that there should be more MD psychiatrists and would like to know how to recruit them. I also think that it would probably be safer for psychologists with extensive training in psychopharmacology to be doing some of the psych prescribing than having general practitioners do it.
There are, in fact, skilled therapists who are not MDs.
And, I don’t wish to engage in ad hominem attacks, but being able to get an MD does not guarantee that someone is bright.
We need more psychiatrists, PCPs and other cognitive specialists. And probably physical therapists too. We have too many interventional cardiologists.
No, allied professionals are part of any service industry, but, do plumbers have non credentialed people come in and do a sizeable portion of their job, just for the plumber to come in and seal a pipe? Do lawyers have their staff go into court and present the introductory comments and then the lawyer starts examining witnesses?
Let’s call this intrusion what it is, as I have noted in the past, everyone thinks they are a psychiatrist and diagnose, prescribe, and then add more drugs, until, they screw up the patient and then push the patient out the door and expect the real expert, me, to undo the damages. And that is the point, psychiatry by a lot of non psychiatrists is now assembly line work, and unfortunately the idiots in my profession who masquerade as leaders and Key Opinion Leaders reinforce this BS.
Also, you can compare somatic care to psychiatry to a point, but, doing labs is not the primary purpose to over 90% of mental health care, so that analogy has overt limits.
You want a start how to recruit more psychiatrists, start by ending the micromanagement by insurance, mental health care administrators, and this growing completely inappropriate intrusions by social workers and psychologists who are telling patients in therapy offices what meds they should be on. Do I tell patients what type of therapy and Axis 4 issues they should be addressing in their therapy treatment during med checks with me 95% of the time, NO. Sometimes I have to offer a point of view, but, ALWAYS tell the patient to discuss it with the therapist. But, I have more and more patients TELLING me what meds they should be on per what an LCSW-C said in an intake. REALLY?!
I don’t get the reference to “being able to get an MD does not guarantee that someone is bright.” Not everyone who is a doctor is reliable and responsible, but, certainly not everyone who is an alleged therapist is capable of providing appropriate therapy, but, we see every day that thinking just hanging up a “shingle” infers an expertise at therapy.
And back to my point in the last comment, WHEN there is a negative outcome in mental health care, who does the patient or family come after first, the therapist who misses the acuity of distress during a session, or the doctor who has to carry 1 Million/3 Million malpractice liability? Even Nurse Practitioners to my knowledge don’t carry sizeable malpractice coverage, yet, they write for meds as much if not more than psychiatrists as a whole.
Again, everyone is a freakin’ psychiatrist until the excrement is coming hard at that fan. And the charlatans are closest to the door and gone, acting so surprised and amazed they should be held accountable.
Hey, been doing this now for 22 years, I have a valid opinion here.
The problem with PCPs “triaging” depression is that they don’t know any way to treat it other than throwing arbitrary prescriptions at it, as though one psychiatric drug is just as good as another and anything might work.
PCPS have been indoctrinated like the rest of the population with drug mythology and are not even as current as psychiatrists (who are terribly behind the times) with the latest information about drug risks.
Also, I’m very uncomfortable with the unitary diagnosis of “depression” for every emotional discomfort. As Mickey described in his anecdote above, very often it’s a life situation that needs to be untangled.
Do lawyers have their staff go into court and present the introductory comments and then the lawyer starts examining witnesses?
You’re not actually advancing your argument here. Paralegals do a lot of work, and most lawyers don’t actually go to court. A lot of lawyers used to do document review, but fewer of them are needed for that kind of mindless work because of advances in IT and search technology.
Doctors, for example, ought to avail themselves of the skills of clinical pharmacists more than most do.
I genuinely do want more psychiatrists. Just complaining about managed care isn’t going to change anything.
Personally, I think that psychiatrists over-identify as physicians when it comes to advocating for what they want. Are surgeons really your natural allies? Back in the day physicians and surgeons were considered different professions. Maybe there was something to the distinction that ought to be brought back.