That brings me to PTSD. Over the years, I saw a number of patients whose current difficulties were born in extreme adversity – what used to be called Traumatic Neurosis. In training, I saw a lot of cases. It was the days of Viet Nam, and the cases filled our VA Hospital. Diagnosis wasn’t a problem since they told us as they walked through the door. But diagnosis of traumatic illness was difficult if the patient [or I] didn’t know they had it. Lenore Terr helped us with that. She identified not symptoms, but signs – things seen over time:
- Trauma specific fears
- Altered states of consciousness
- Repetitive experience – eg reinactments
- An altered view of the self and the world
-
Trauma specific fears: Patients with PTSD have unusual fears, often very odd things or more often situations. Those fears are specific to the specific trauma they experienced. Even if it’s a common fear like acrophobia, it will have specificity, "I might jump."
-
Altered states of consciousness: Patients with PTSD have dissociative episodes, but they too have specificity. They ‘zone out’ in particular settings, ones that reproduce their traumatic moments more or less exactly.
-
Repetitive experience – eg reinactments: PTSD patients have repetitive experience, dreams, fantasies, patterns. Again specific to the trauma.
- An altered view of the self and the world: The PTSD patient feels broken. In many ways they are correct. They’ve had something happen that has overwhelmed the mind, and so they know that can happen – an indelible knowledge.
Allele-specific FKBP5 DNA demethylation mediates gene–childhood trauma interactions
by Torsten Klengel, Divya Mehta, Christoph Anacker, Monika Rex-Haffner, Jens C Pruessner, Carmine M Pariante, Thaddeus W W Pace, Kristina B Mercer, Helen S Mayberg, Bekh Bradley, Charles B Nemeroff, Florian Holsboer, Christine M Heim, Kerry J Ressler, Theo Rein, and & Elisabeth B Binder
Nature Neuroscience. doi:10.1038/nn.3275. Published online 02 December 2012
AbstractAlthough the fact that genetic predisposition and environmental exposures interact to shape development and function of the human brain and, ultimately, the risk of psychiatric disorders has drawn wide interest, the corresponding molecular mechanisms have not yet been elucidated. We found that a functional polymorphism altering chromatin interaction between the transcription start site and long-range enhancers in the FK506 binding protein 5 (FKBP5) gene, an important regulator of the stress hormone system, increased the risk of developing stress-related psychiatric disorders in adulthood by allele-specific, childhood trauma–dependent DNA demethylation in functional glucocorticoid response elements of FKBP5. This demethylation was linked to increased stress-dependent gene transcription followed by a long-term dysregulation of the stress hormone system and a global effect on the function of immune cells and brain areas associated with stress regulation. This identification of molecular mechanisms of genotype-directed long-term environmental reactivity will be useful for designing more effective treatment strategies for stress-related disorders.
These are subjects recruited from the waiting rooms [not psychiatry waiting rooms] and from city bus ads in urban Atlanta, a population well known to me. They’ve been given questionnaires about their past, their symptoms, donated DNA samples, and been paid for their time. Here’s a video of Dr. Nemeroff’s presentation of this paper at an NYU Grand Rounds earlier this year:
[click the graphic to see a video of Dr. Nemeroff’s presentation]
Everything below the first bullet as you read down this summary slide is hypothesis at best. In both the paper and this video, they are presented not as increasingly speculative hypotheses verging on the realm of Jules Verne, Robert Heinlein, and Isaac Asimov, but as established facts. His thinking hinges on the concept of epigenetics, ways of inheritance other than through hard wired DNA sequences – a fascinating, leading edge area of study, but hardly up to this kind of extrapolation.
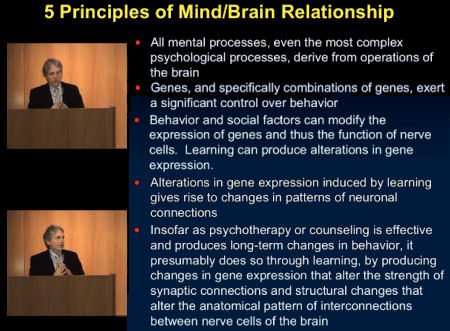
I try to stick to criticisms based on scientific misadventure with my endless graphs and quotes, but here I’m staying on the surface. Just my conclusion. I don’t really believe this. I don’t think that abuse, deprivation, or trauma go back down the pipeline to the DNA or whatever epigenetic mechanisms are around and biologically make changes that make us sick depending on our genetics. I know abuse, deprivation, or trauma can make us sick, but not like this. I’m completely sure that’s not the reason PTSD persists throughout life. And with PTSD, it’s not diagnosed by questionnaire. It’s a diagnosis best made by a careful history, taken over time, defining the unique mental illness created by the specific idiosyncratic circumstances of a person. Everything here beyond [1] mental phenomena happen in the brain and [2] bad early experiences portend trouble down the road [both general knowledge] is speculation – and wild speculation at that. I’ll even go out on a limb. In my 40 year history as a psychiatrist doing psychotherapy, I’ve had my share of successes, but I guarantee it wasn’t "by producing changes in gene expression that alter the strength of synaptic connections and structural changes that alter the anatomical pattern of interconnections between nerve cells of the brain." Not once.
This is what happens when people follow cookie cutter procedures in clinical research. Such people don’t understand the nuances of PTSD or of the diagnostic process, as you say. The basic experiments in this report are probably okay, but the clinical side of the work is weak, especially in relation to the expansive claims about clinical issues.
Here is a link to another recent discussion on the Nature News blog of reports from this Emory group. Follow the comments thread. There are further critiques of their work at PubMed ID 21893663 (Posttraumatic stress disorder subtypes invalid) and PubMed ID 19892206 (Trauma and mental health in U.S. inner city populations).
Is this a good use of scarce NIMH funds or is it another case of NIMH capture by academic impresarios? You be the judge. Where are the grownups at NIMH?
Did Dr. Collins of NIH ever respond to Senator Grassley’s letter?
The assumption that all PTSD is the same, as if it were the result of traumatic stress pushing a button in the brain marked PTSD, is the most specious aspect of the biological lens in my book. In the eighties there were support groups for women who had been sexually abused as children in which there was always that woman who couldn’t remember anything about being sexual abused, but a psychiatrist had told her she was. Everyone but that woman is trying to forget it while she tried to remember (something that probably didn’t happen to her) and that woman always appeared to be an alcoholic.
For veterans, how could the traumatic stress of being in a combat situation and being the perpetrator of violence be the psychological equivalent of being raped? PTSD is exceedingly psychological.