Cochrane signs up to AllTrials initiative to campaign for registration and reporting of all clinical trials
Cochrane Collaboration
Press Release
April 19 , 2013The Cochrane Collaboration, the international not-for-profit organization that produces systematic reviews of healthcare evidence and the largest database of randomized controlled trials, published online in The Cochrane Library, has today formalized its commitment to the AllTrials: All Trials Registered | All Results Reported initiative to campaign for the registration and reporting of all clinical trials.
The AllTrials campaign aims to draw attention to the crisis of unreported trial data. Hundreds of thousands of clinical trials have been conducted from which no or limited data have been made available; data critical to enabling doctors and regulators to make informed decisions about which treatments to use and fund. This is a serious problem for evidence-based healthcare researchers including The Cochrane Collaboration, because all the evidence about a treatment is needed to understand its risks and benefits. Without a complete picture of trial results available, information is lost; bad treatment decisions may be made; financial investment into ineffective treatments are approved by governments and regulators; opportunities for better and more effective treatment are missed; and trials are repeated unnecessarily, duplicating effort and wasting resources.
AllTrials was launched in January 2013 by Ben Goldacre, bestselling author, broadcaster and medical doctor, whose exposé on scientific inaccuracy Bad Science [2008] reached #1 in the UK paper back non-fiction charts; along with the charity Sense About Science; the Centre for Evidence Based Medicine in Oxford; the James Lind Initiative; and the BMJ. In the three months since its inception, AllTrials has gathered more than 47,000 signatures for its petition calling on governments, regulators and research bodies to implement trial registration and reporting measures; as well as the support of hundreds of organizations and institutions working in research, patient advocacy and health care. The Cochrane Collaboration was one of the earliest organizations to offer support, and to further demonstrate its commitment to the goals of the AllTrials initiative, has today formalized its involvement as one of the initiative’s principal supporters and organizers…
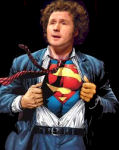 Six months ago, I followed some links sent by Altostrata to a Ted Talk by a guy I’d never heard of named Ben Goldacre [something of value…]. Like most, I was captivated by his playful style and obvious mastery of his science [evidence-based medicine]. I didn’t like the term [still don’t], but I sure liked him and what he had to say. It was there I first heard of "funnel plots" and first thought correctly about the real impact of all the missing trials. The month before, I had happened upon the raw data from the infamous Paxil Study 329 posted shortly before without fanfare [a movement…]. And I realized that with no special expertise or tools bigger than an Open Office Spreadsheet, I could easily confirm that it was as big a piece of distorted science as we all thought. But I guess I was still under some kind of spell and it didn’t really sink in that all clinical trial data really ought to be open access until I heard Ben say it in such a matter of fact way. Three months later, there were two new books on my shelf [Bad Science and Bad Pharma] and the All·Trials petition was launched [click it and sign it…]. Now it’s a movement, a story with legs as they say in media-talk. One can legitimately hope that it will lead us to some kind of actual reform. Today, the prestigious Cochrane Collaboration officially signs on as a sponsor.
Six months ago, I followed some links sent by Altostrata to a Ted Talk by a guy I’d never heard of named Ben Goldacre [something of value…]. Like most, I was captivated by his playful style and obvious mastery of his science [evidence-based medicine]. I didn’t like the term [still don’t], but I sure liked him and what he had to say. It was there I first heard of "funnel plots" and first thought correctly about the real impact of all the missing trials. The month before, I had happened upon the raw data from the infamous Paxil Study 329 posted shortly before without fanfare [a movement…]. And I realized that with no special expertise or tools bigger than an Open Office Spreadsheet, I could easily confirm that it was as big a piece of distorted science as we all thought. But I guess I was still under some kind of spell and it didn’t really sink in that all clinical trial data really ought to be open access until I heard Ben say it in such a matter of fact way. Three months later, there were two new books on my shelf [Bad Science and Bad Pharma] and the All·Trials petition was launched [click it and sign it…]. Now it’s a movement, a story with legs as they say in media-talk. One can legitimately hope that it will lead us to some kind of actual reform. Today, the prestigious Cochrane Collaboration officially signs on as a sponsor.  As much as I’m interested in knowing how these recent events and Ben’s particular style became the kindling that finally seems to have ignited a blaze so long overdue, I’m even more interested in how we got this far off of the track in the first place. When I arrived in medical school, I fell in love with the literature. I had been a product of that post-Sputnik age where the only question was what kind of scientist were you going to be and had lived a life surrounded by text-books, but the medical literature was so much more. It came weekly or monthly, and you could even sometimes feel science moving. Later, in a fellowship, I was involved in a project that involved looking back through the old literature with a new idea to see if its roots were previously apparent – and they were. They had been dutifully recorded for years, awaiting our data from a new electron microscope technique to make sense of a piece of it. I couldn’t imagine anything more interesting than that kind of continuity.
As much as I’m interested in knowing how these recent events and Ben’s particular style became the kindling that finally seems to have ignited a blaze so long overdue, I’m even more interested in how we got this far off of the track in the first place. When I arrived in medical school, I fell in love with the literature. I had been a product of that post-Sputnik age where the only question was what kind of scientist were you going to be and had lived a life surrounded by text-books, but the medical literature was so much more. It came weekly or monthly, and you could even sometimes feel science moving. Later, in a fellowship, I was involved in a project that involved looking back through the old literature with a new idea to see if its roots were previously apparent – and they were. They had been dutifully recorded for years, awaiting our data from a new electron microscope technique to make sense of a piece of it. I couldn’t imagine anything more interesting than that kind of continuity.
I personally left the thread of the contemporary psychiatry literature thirty years ago. Maybe I should say it like it felt. It felt like it left me as it became rapidly and monotonously biologified after 1980, and I was focused on other things. But coming back to it in recent years, I’m afraid that my attitude of wonder has changed. I don’t trust it anymore, or the process that creates it. In former days, there was plenty that I thought was wrong, but not wrong on purpose. There are so many clinical trials that are misrepresented. All the old graphs, tables, and statistics are there, but they have to be read in a different way. After the title, the next most important parts are the funding source, the acknowledgements, the disclosures, the authors’ affiliations (and worse, there was a period where that information wasn’t even available). Beside the monotonous trials, there were reviews and perspectives that were thinly disguised commercials. And in the psychiatric literature, there has been an absence – a dirth of a medical skepticism that I’d become used to. Everything was just great. My impression is that this b.s. factor in the psychiatric literature is unique, or at least much more prevalent than elsewhere in medicine.
So as we move forward hopefully with a new resolve to make our scientific literature actually scientific, I think we’re duty-bound to figure out why it hasn’t been for such a long time. Why would the JAACAP publish Paxil Study 329 over the objections of the peer reviewers? Why, in light of the abundant available evidence would the editor refuse to retract it even now? Why would a terminally flawed meta-analysis like that published in the Archives of General Psychiatry last year by Robert Gibbons et al be published at all, or still be there? Why would a requirement to publish trial results on clinicaltrials.gov within a year of a trial’s completion be ignored most of the time with no apparent consequences?
As long as most research is funded privately (even at public institutions) “we” start with soliciting.
Great post all the way around.
This especially stands out:
“When I arrived in medical school, I fell in love with the literature. I had been a product of that post-Sputnik age where the only question was what kind of scientist were you going to be and had lived a life surrounded by text-books, but the medical literature was so much more. It came weekly or monthly, and you could even sometimes feel science moving. Later, in a fellowship, I was involved in a project that involved looking back through the old literature with a new idea to see if its roots were previously apparent – and they were. They had been dutifully recorded for years, awaiting our data from a new electron microscope technique to make sense of a piece of it. I couldn’t imagine anything more interesting than that kind of continuity.”
Beautifully put.
The marketing of junk science to sell ineffective & dangerous drugs for huge profits never ceases. If it’s not the chemical imbalance myth…then it’s the recycled gene theory… Today’s Biological Psychiatry has little to do with medicine or health…Yet, it has everything to do with institutionalized greed and power…
The pharmaceutical industry sponsored Propaganda —> http://blogs.psychcentral.com/bipolar/2013/04/antipsychotics-gene-function-bipolar/
I think your bring up the larger question of how to change organized medicine in general and psychiatry in particular. It seems that fewer and fewer doctors are choosing to join the AMA or APA, which is certainly one option. However, I wonder if change could effectively be made from within. For example, I recall readingthis NYTimes article from a couple of years ago that looks at how state medical associations are changing, becoming less conservative as more women become doctors and more doctors join hospital-based practices rather than owning private practices. Could something similar happen with the APA, as more young psychiatrists become disillusioned with the academic-pharma complex?
psycritic.blogspot.com
In the larger sense, it’s necessary to recgonize that all science is conducted in the service of an agenda. Sometimes it’s a flagrant and obvious agenda, sometimes it’s hidden, and sometimes the “agenda” is nothing more than a simple hypothesis (which is what we want).
Something else that’s worth thinking about is that the roots of science are in storytelling. Thousands of years ago, storytelling was the only tool mankind had for making sense of the natural universe. We still love stories. It’s in our blood to love a good story. In science, the Theory is the unit of storytelling. The best-accepted theories are the ones that tell the most satisfying story. They can be satisfying because they fit the facts, or for any number of other reasons. But basically, scientists are in the story-weaving business. A good theory always also makes a good story, and that’s part of why so many bad ideas in science are so hard to give up, why people cling to theories that should have died long ago: People love a good story.
Sadly, the pharma industry has learned these lessons only too well. They are experts in conjuring well-crafted stories, stories we WANT to believe, then dressing them in the silk robes of science. The understand the Cult of Story. It’s a powerful cult, one we will not soon rid ourselves of as a species.
These are good observations. A classic ‘story’ in biological psychiatry was the monoamine theory of depression. It served for decades the function that Thomas Kuhn called heuristic: it provided a platform for new and more incisive questions. It was also a convenient vehicle for the ‘agenda’ of attracting research dollars to the field. In its day it was an absolutely respectable theory, qua theory, but it was eventually reified and then hijacked for other agendas long after the paradigm was exhausted.
Kas,
Very nice comment.
If you haven’t seen these 2 related posts you might find them of interest:
http://blogs.discovermagazine.com/neuroskeptic/2013/03/01/were-all-jonah-lehrer-except-me/
(including a very nice comment from Ed Yong – the first one in the comments section – where he says “Selling attractive narratives at the expense of interesting truths. And that’s really the issue here.”)
And
http://neuroself.com/2011/05/29/jonah-lehrer-is-not-a-neuroscientist/
http://www.bmj.com/content/346/bmj.f2336
On one hand:
“My consultant recently told me that no trials had been done to determine what the minimum effective dose of adalimumab was, nor would there likely ever be; a drug company has no interest in showing you can take less of something.”
Something it would seem that randomized blinded trials (preferably embedded into standard care settings) might do uniquely well.
On the other hand:
“Since I started taking adalimumab I have the least symptoms since diagnosis. I am no longer taking steroids; I have started to recover from 15 years of side effects; and I spend less time in clinical care and off work on sick leave.
However, anecdotes are not the foundation of evidence based medicine,”
Does this mean that his regimen should not be covered if the meta-analysis of all the RCTs that were done are not statistically significant?
“Because he’s a physician, Wennberg was able to sit down with surgeons and try to get them to explain how they decided surgery was necessary in a given case. What he found was that the decision rules used by one surgeon were totally different from, and sometimes contradictory to, another surgeon’s rules. In the course of trying to understand all of this, he stumbled across a forgotten study looking at referrals for tonsillectomy in New York City schools. When 400 children were examined, half were felt to need a tonsillectomy. When those not referred were blindly re-examined, another 40% were referred for the procedure. For the kids rejected twice, and again blindly re-examined, another 44% were recommended. In short, referral seemed to driven not by any objective reason but a belief that half of all children seen should be referred!! This is what passes for medical science?”
http://www.amazon.com/review/R201QWX9TKFFYO/ref=cm_cr_dp_title?ie=UTF8&ASIN=0199731780&channel=detail-glance&nodeID=283155&store=books
Highly Relevant to the discussion above:
http://www.huffingtonpost.com/marilyn-wedge-phd/science-rhetoric-and-the-_b_3024083.html
From a series of commentaries on this:
http://www.huffingtonpost.com/ben-goldacre/prescription-drugs_b_3018272.html
Other of the commentaries that stood out:
http://www.huffingtonpost.com/wray-herbert/revisiting-the-placebo_b_3006277.html
&
http://www.huffingtonpost.com/anthony-g-greenwald/publication-bias-is-a_b_3017845.html
&
http://www.huffingtonpost.com/claire-mccarthy-md/medical research_b_3033530.html
The remainder of the posts:
http://www.huffingtonpost.com/ida-sim-md-phd/medicines-hard-drive-is_b_3019907.html
http://www.huffingtonpost.com/martha-rosenberg/when-the-publication-plan_b_3023945.html
http://www.huffingtonpost.com/brian-secemsky/a-push-to-publish_b_3020293.html
http://www.huffingtonpost.com/dr-peter-breggin/be-skeptical-of_b_3020841.html
http://www.huffingtonpost.com/dr-dennis-gottfried/its-not-working_b_3052674.html
http://www.huffingtonpost.com/toni-miller/getting-past-the-idea-of-_b_3017911.html
http://www.huffingtonpost.com/claire-mccarthy-md/medical-research_b_3033530.html
The fixed link from above
The first link above on rhetoric ties in with another of Kas’ earlier comments. In that link she says:
“Even though family therapy, unlike many psychiatric drugs, can do no harm,…”
Interesting to think about that statement in the context of:
http://asserttrue.blogspot.com/2013/04/when-psychotherapy-goes-wrong.html
“Why is publication bias so remarkably difficult to fix? It’s because all actors in the research-publication system have reasons (not necessarily commendable ones) for preferring the present flawed system.”
The corollary question is: why are clinicians by and large seemingly so unconcerned about publication bias?