PLoS Medicineby Yasmina Molero, Paul Lichtenstein, Johan Zetterqvist, Clara Hellner Gumpert, and Seena FazelSeptember 15, 2015
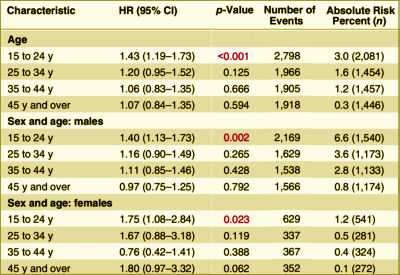
Background: Although selective serotonin reuptake inhibitors [SSRIs] are widely prescribed, associations with violence are uncertain.Methods and Findings: From Swedish national registers we extracted information on 856,493 individuals who were prescribed SSRIs, and subsequent violent crimes during 2006 through 2009. We used stratified Cox regression analyses to compare the rate of violent crime while individuals were prescribed these medications with the rate in the same individuals while not receiving medication. Adjustments were made for other psychotropic medications. Information on all medications was extracted from the Swedish Prescribed Drug Register, with complete national data on all dispensed medications. Information on violent crime convictions was extracted from the Swedish national crime register. Using within-individual models, there was an overall association between SSRIs and violent crime convictions [hazard ratio [HR] = 1.19, 95% CI 1.08–1.32, p < 0.001, absolute risk = 1.0%]. With age stratification, there was a significant association between SSRIs and violent crime convictions for individuals aged 15 to 24 y [HR = 1.43, 95% CI 1.19–1.73, p < 0.001, absolute risk = 3.0%]. However, there were no significant associations in those aged 25–34 y [HR = 1.20, 95% CI 0.95–1.52, p = 0.125, absolute risk = 1.6%], in those aged 35–44 y [HR = 1.06, 95% CI 0.83–1.35, p = 0.666, absolute risk = 1.2%], or in those aged 45 y or older [HR = 1.07, 95% CI 0.84–1.35, p = 0.594, absolute risk = 0.3%]. Associations in those aged 15 to 24 y were also found for violent crime arrests with preliminary investigations [HR = 1.28, 95% CI 1.16–1.41, p < 0.001], non-violent crime convictions [HR = 1.22, 95% CI 1.10–1.34, p < 0.001], non-violent crime arrests [HR = 1.13, 95% CI 1.07–1.20, p < 0.001], non-fatal injuries from accidents [HR = 1.29, 95% CI 1.22–1.36, p < 0.001], and emergency inpatient or outpatient treatment for alcohol intoxication or misuse [HR = 1.98, 95% CI 1.76–2.21, p < 0.001]. With age and sex stratification, there was a significant association between SSRIs and violent crime convictions for males aged 15 to 24 y [HR = 1.40, 95% CI 1.13–1.73, p = 0.002] and females aged 15 to 24 y [HR = 1.75, 95% CI 1.08–2.84, p = 0.023]. However, there were no significant associations in those aged 25 y or older. One important limitation is that we were unable to fully account for time-varying factors.Conclusions: The association between SSRIs and violent crime convictions and violent crime arrests varied by age group. The increased risk we found in young people needs validation in other studies.
[cropped to fit the space]
Besides having access a cohort of 8+M people [~10% on SSRIs] with their prescription records and the public records of every brush with the law, they had some mighty fine computers and statisticians to have extracted their data and cross-checked so many covariates. I couldn’t possibly"vet" all of their analyses. But the core thread is that they isolated periods when patients were "on" SSRIs and when they were "off" the medication, and they compared the arrest rates for violent crimes "on" and "off" – deriving a Hazard Ratio.
-
Gibbons RD, Hur K, Bhaumik DK, Mann JJ.Arch Gen Psychiatry. 2005 Feb;62(2):165-72.
-
Gibbons RD, Hur K, Bhaumik DK, Mann JJ.Am J Psychiatry. 2006 Nov;163(11):1898-904.
-
Charles B. Nemeroff, Amir Kalali, Martin B. Keller, Dennis S. Charney, Susan E. Lenderts, Elisa F. Cascade, Hugo Stephenson, and Alan F. SchatzbergArch Gen Psychiatry. 2007 Apr;64(4):466-472.
-
Nakagawa A, Grunebaum MF, Ellis SP, Oquendo MA, Kashima H, Gibbons RD, Mann JJ.J Clin Psychiatry. 2007 Jun;68(6):908-916.
-
Benji T. Kurian, MD, MPH; Wayne A. Ray, PhD; Patrick G. Arbogast, PhD; D. Catherine Fuchs, MD; Judith A. Dudley, BS; William O. Cooper, MD, MPHJAMA: Pediatrics. 2007 Jun;161(7):690-696.
-
Gibbons RD, Brown CH, Hur K, Marcus SM, Bhaumik DK, Mann JJ.Am J Psychiatry. 2007 Jul;164(7):1044-1049.
-
Early evidence on the effects of regulators’ suicidality warnings on SSRI prescriptions and suicide in children and adolescents. [see peaks and valleys…]Gibbons RD, Brown CH, Hur K, Marcus SM, Bhaumik DK, Erkens JA, Herings RM, Mann JJ.Am J Psychiatry. 2007 Sep;164(9):1356-1363.
-
Brown CH, Wyman PA, Brinales JM, Gibbons RD.Int Rev Psychiatry. 2007 Dec;19(6):617-631.
-
Gibbons RD, Segawa E, Karabatsos G, Amatya AK, Bhaumik DK, Brown CH, Kapur K, Marcus SM, Hur K, Mann JJ.Stat Med. 2008 May 20;27(11):1814-1833.
-
Barry CL and Busch SH.Pediatrics. 2010 125[1]:88-95.
-
Gibbons RD, Mann JJ.Drug Saf. 2011 May 1;34(5):375-395.
-
Susan Busch, Ezra Golberstein, Ellen MearaNATIONAL BUREAU OF ECONOMIC RESEARCH, September 2011.
-
Robert D. Gibbons, Hendricks Brown, Kwan Hur, John M. Davis, and J. John MannArch Gen Psychiatry. 2012 Jun;69(6):580-587.
-
Gibbons RD, Coca Perraillon M, Hur K, Conti RM, Valuck RJ, and Brent DAPharmacoepidemiologic Drug Safety. 2014 Sep 29. doi: 10.1002/pds.3713. [Epub ahead of print]
-
Christine Y Lu, Fang Zhang , Matthew D Lakoma analyst, Jeanne M Madden, Donna Rusinak, Robert B Penfold, Gregory Simon, Brian K Ahmedani, Gregory Clarke, Enid M Hunkeler, Beth Waitzfelder, Ashli Owen-Smith, Marsha A Raebel, Rebecca Rossom, Karen J Coleman, Laurel A Copeland, Stephen B SoumeraiBMJ. 2014 348:g3596.
-
PSYCHIATRICNEWSby Mark Moran12/30/2014
-
by Richard A. Friedman, M.D.New England Journal of Medicine 2014 371:1666-1668.
-
by Marc B. Stone, M.D.New England Journal of Medicine 2014 371:1668-1671.
-
New York Timesby Richard A. FriedmanAUGUST 3, 2015
i think actually we have seen enough of these Swedish studies (even if the conclusions in this one fit with the data in RCTs) It’s just to take a look at the studies by Goran Isacsson over the years, using Swedish registers to “prove” his ideas about antidepressants as miracle drugs protecting against suicide.
As for Lichtensten and his earlier study saying that ADHD drugs are protecting against criminality we can say that it is about the same. See Lichtenstein. “Medication for attention-deficit hyperactivity disorder and criminality.” and the words by Whitaker about it (page 30) http://www.humanact.se/laddaner_files/Medicating%20ADHD.pdf
In our N=1 we definitely saw an emergence of new aggressive behaviors which began around 3 months after an SSRI was added. However these aggressive behaviors first worsened during the first month or two after stopping the antidepressant, and then slowly diminished over a period of about a year after the SSRI was stopped (and are now completely gone ). We have wondered whether these behaviors were related to the SSRI, but if they were, this on /off study design wouldn’t have picked up this information because of the length of time it took for the behaviors to diminish. I realize that in this study the adolescents would have been on ONLY an antidepressant (not an antidepressant with an antipsychotic), but I am wondering how the ‘off’ periods were measured. Do you know if the ‘off’ periods would have been measured right away on the next day the antidepressant was stopped, or after a couple of months of discontinuing the antidepressant or what?
Sally,
It’s a great question. I looked for the answer first time around, and couldn’t determine the answer, but I’ll give it another look..
Olov>>> is Another typical Swedish name, just as my name Ove. If you happen to be professional in Swedish psychiatry or the victim of the same. Then I’m very interested in getting in Contact. I have had a hard time finding anyone who dares to criticize psychiatry and/or psychiatric drugs in sweden.
As for this research: I’m in brief Contact with one of the scientists to try to work out whether I’m a part of the statistics they’ve used.
I’m curious whether they limit the on/off period also to 2006-2009, because that excludes me. But I was sentenced to prison during that period, and I sure as “H” was on Paxil. But my “off-period” was Before 1998. I’m still on it, my one try to wean off ended in disaster.
I’m hooked on a drug that the manufacturer have to use “statistical curiosities” to find “efficacious and well tolerable”.
Ove,
For some, getting off the short acting SSRIs can indeed be a nightmare. If you haven’t already found SurvivingADs or Bob Fiddaman‘s blog, both are worth a look.
#17 Antidepressants’ Black-Box Warning
– 10 Years Later
by Richard A. Friedman, M.D.
New England Journal of Medicine 2014 371:1666-1668.
In #17, Friedman falsely states that there were no completed suicides in Stone et al., 2009,. He doesn’t name the study, the year, or Stone, and links to a different study.
Friedman used essentially the same paragraph in a post-Germanwings Q&A in the NYTimes. Again, he said there were no suicides, didn’t name the study, the year, or the authors, and gave no reference at all.
http://well.blogs.nytimes.com/2015/03/30/ask-well-depression-and-its-risks/?_r=0
The NYTimes corrected the misstatement upon receipt of a letter from a reader two months ago. NEJM did not.
Friedman got the number of studies in the meta-analysis right (372), but not the number of dead (8). Five were in treatment groups and 3 were in placebo groups. Stone (an FDA employee) et al. had a funny way of describing the finding:
“The odds ratio for completed suicide (2.13) was higher for those treated with an antidepressant, but this was based on just eight events and was not significant (0.41 to 10.99)”
http://www.bmj.com/content/339/bmj.b2880
(Risk of suicidality in clinical trials of antidepressants in adults: analysis of proprietary data submitted to US Food and Drug Administration)
@Sally, that is a good question. You should post a comment on the PLOS article’s web site and see if the authors will provide a response.
Sally,
I agree with A. Tasso. I read it a second time around, both times, looking for that particular information, I just couldn’t tell.
Thanks Sally (and Mickey!) for reading the fine print on this! Hope we can get an answer. I do think their approach of comparing the subjects on SSRIs to them-selves is an interesting idea — much more meaningful than population studies.
It is subject to bias *in favor of* treatment, especially if the treaters are involved in the research. A couple of recent studies cranked out by John Kane’s Abilify Maintena Machine used this approach, dubbed a “mirror image” study. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3709884/ Since the only people who got shots were those who did badly on pills, they couldn’t help but show progress. However, if the treatment changes were not undertaken for research purposes, and you’re looking at the results from arm’s length, it should be pretty good.
Certainly the unquestioned gospel of all nonprofit and professional groups is that the way to prevent crime and violence in young people (not to mention self-harm) is to GET THEM INTO TREATMENT. Very sobering if that turned out to be a bad move, looking back …
I too was extremely interested in the Swedish SSRIs and Violent Crime: A cohort study. And having subjects as their own control definitely beats a lot of the problems with population studies. Thanks for posting the data table, I do not have access to anything but the abstract (which was quite thorough). One of the best things about your posts is that you always provide good detail (and pictures!). I had the same question as Sally about withdrawal, but I also wonder if something gets missed by using regression analysis on a population that is not homogeneous w.r.t. susceptibility to the drug influence. What if some non-metabolizers (a small group percentage-wise) are much more likely to become violent, while others see their risk of violence reduce? This is a real possibility. This in no way makes the conclusions wrong (the association between SSRIs and violent crime convictions and violent crime arrests varied by age group) but the potential off-setting impact of these differently reacting individuals might be hiding an important effect.