-
completed Safety and Tolerability Study of Lu AF35700 After Repeated Dosing in Patients With Schizophrenia [96 subjects]
-
recruiting Effect of Lu AF35700 in Patients With Treatment-resistant Schizophrenia [964 subjects]
FiercePharmaBy Nick Paul TaylorMarch 17, 2016Lundbeck has started the first of several planned Phase III trials of its candidate against treatment-resistant schizophrenia, Lu AF35700. The candidate is a key component of the turnaround strategy initiated by Kåre Schultz, who has shed other pipeline prospects in order to up Lundbeck’s bet on Lu AF35700 since taking over as CEO last year.
Copenhagen, Denmark-based Lundbeck is kicking off the pivotal trial program of the experimental drug with a Phase III study that will recruit 1,000 patients across 15 countries. In the study, Lundbeck will administer one of two doses of Lu AF35700 to patients with treatment-resistant schizophrenia. If the drug works as Lundbeck hopes, participants’ scores on the Positive and Negative Syndrome Scale [PANSS] will improve following 10 weeks of treatment. The primary PANSS endpoint is being supplemented with Clinical Global Impression – Severity of Illness scores and Personal and Social Performance Scale data.
Lundbeck expects to be running the study for the next three years, during which time it will roll out additional trials with a view to gathering data on more than 2,000 people with treatment-resistant schizophrenia. The size of the bet is proportional to Lundbeck’s assessment of the scale of the unmet need and opportunity associated with treatment-resistant schizophrenia. "Today there is only one therapy approved for patients with treatment-resistant schizophrenia, and its use is severely limited by its problematic safety profile," Lundbeck R&D Chief Anders Gersel Pedersen said in a statement…
FiercePharmaBy Nick Paul TaylorAugust 20, 2015Lundbeck has initiated a rejig of its pipeline, taking an ax to undisclosed early-stage assets in order to funnel cash into what it sees as its most promising candidates. The schizophrenia drug Lu AF35700 is among the beneficiaries of the reshuffle, with Lundbeck using its reorganized balance sheet to advance the therapy through development unpartnered.
Copenhagen, Denmark-based Lundbeck unveiled the tweaks to its R&D priorities alongside sweeping changes to its operations, which will see it shed 1,000 jobs in an attempt to become profitable. The commercial operation is expected to bear the brunt of the cuts but R&D will be affected, too, with recently-appointed CEO Kåre Schultz committing to dropping certain early-stage assets. Trimming the pipeline will allow Lundbeck top focus its cash on programs in which it thinks it has the clearest understanding of the underlying science, such as the schizophrenia drug Lu Af35700.
"35700 is an antipsychotic with a profile that is somewhat different than most drugs available. What we see is that many of the drugs that are available on the market today are predominantly driving effects through D2," Lundbeck R&D chief Anders Gersel Pedersen said on a conference call. 35700, like clozapine, has a strong binding affinity to the D1 receptor. Lundbeck hopes to differentiate its pipeline candidate from clozapine through its side effect profile, giving patients who are resistant to D2-targeted drugs a treatment option that doesn’t cause weight gain and metabolic disturbances. Lundbeck’s belief in this hypothesis has led it to conclude Lu Af35700 is among its most promising early-stage assets. "We have to put our bets where we think we have the best ability to translate science into products," Pederson said…
The FDA doesn’t have to follow the advice of its expert review panels, but it usually does. That’s a standard line in stories about advisory committee votes. Unfortunately for Lundbeck and Takeda, their new Brintellix app is one of the unlucky ones.
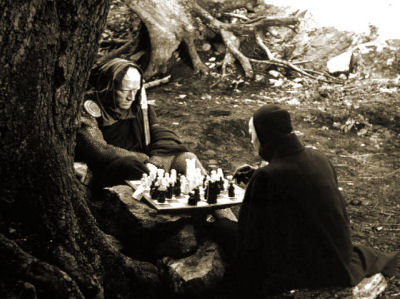 I doubt most of us would say it that way ["unlucky"]. There was a surprising-to-me absence of attention to the actual medical benefit or risk – mainly comments on success or failure of various gambits. I’m not being hyper-moral here, business sites are about business after all. It was just a bit jarring – as was something else. Much of this literature is about strategies. It reads like a huge chess game with the various moves and gambits cataloged, and sometimes relished. In the case of Lu AF35700, Lundbeck’s new CEO, Kåre Schultz, is shutting down some of Lundbeck’s R&D, laying off employees, and dropping other candidate drugs to raise the cash for his big bet on Lu AF35700 [AKA rejig]. A 1000 Subject three year International Clinical Trial is apparently going to cost them a mint. Just like the failed bet they made on Brintellix® to be a think-better antidepressant cost them dearly. It’s little surprise they hauled in the uber-KOLs for that FDA hearing.
I doubt most of us would say it that way ["unlucky"]. There was a surprising-to-me absence of attention to the actual medical benefit or risk – mainly comments on success or failure of various gambits. I’m not being hyper-moral here, business sites are about business after all. It was just a bit jarring – as was something else. Much of this literature is about strategies. It reads like a huge chess game with the various moves and gambits cataloged, and sometimes relished. In the case of Lu AF35700, Lundbeck’s new CEO, Kåre Schultz, is shutting down some of Lundbeck’s R&D, laying off employees, and dropping other candidate drugs to raise the cash for his big bet on Lu AF35700 [AKA rejig]. A 1000 Subject three year International Clinical Trial is apparently going to cost them a mint. Just like the failed bet they made on Brintellix® to be a think-better antidepressant cost them dearly. It’s little surprise they hauled in the uber-KOLs for that FDA hearing. I hadn’t thought of it before, and maybe it was The Big Short movie that had me in this frame of mind, but a lot of the investing in pharmaceuticals is analogous to the Commodities Market – betting on a future value. Again, the pipeline paradigm, as in being in a position to reap large profits when and if the product flows out into the market. I suppose any business venture is like that, but here, it’s in bas relief because of the long development process, the FDA’s yes/no position, the guaranteed time limited monopoly afforded by the patent/exclusivity laws, and the presence of those pesky middlemen [AKA physicians]. So if Lu AF35700 turns out as they hope [a non-toxic Clozaril], as things now stand, they’ll be able to charge Gilead/Valeant/Shkreli prices – the treatment-resistant Schizophrenia patients are unlikely to have very deep pockets, so I presume they’re aiming at third patry payers.
I happened to meet Matthew Herper from Forbes a while back. If you haven’t run across his site, you might find his reporting of interest:
http://www.forbes.com/sites/matthewherper/#7797f6932b5f
Given recent events, the Shkreli/Valeant model may be permanently broken.
Some of these new cancer drugs are 100-150 K a year commitments.
If something can’t possibly continue to go on it won’t.
The whole 2 billion dollars in R&D/15 years of approval then charge anything you want model has to be revisited and reformed. Boomers are starting to die in large numbers and I don’t think they will stand for it.
Right… and a key variable is the added value for the $$$.
Many of the Valeant drugs (as with Shrekli’s Turing Pharmaceuticals) are old drugs that had been very inexpensive, bought by the “entrepreneurs,” and then prices hiked astronomically — with no drug development costs.
The model was sheer economic opportunism in market niches where there was no competition.
That’s the point… no added value.
Shkreli and Valeant aside, lately PhRMA have been beating the drum for outcomes based pricing. That’s how bio-pharma tries to justify astronomical pricing. Even if their overstated claims for outcomes – usually expressed in Quality Adjusted Life Years or QALYs – were true, pricing does not necessarily follow. An ethical basis for pricing would be cost of development, manufacture, and distribution. Consider pricing by physicians. They don’t get differential pricing based on outcomes but on clinical encounters. The PhRMA talk is just self-interested woo woo.