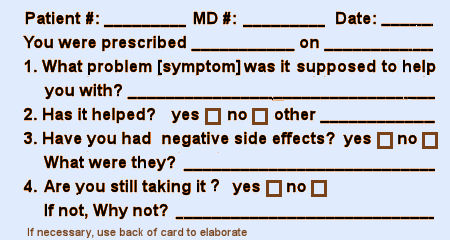
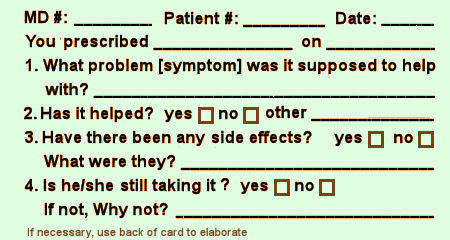
I don’t much like questionnaires. But if required, I prefer yes/no or one word answer questions. And I’ve never designed a questionnaire [before today]. But as I was thinking about post-approval monitoring, I decided I’d give it a shot. I was thinking about what information you might gather post approval in help seeking patients taking the drug. You wouldn’t much care about controls, or statistical medicinal properties. You’d want to know what a clinician would want to know – is it helping? any problems? And how would one gather such information?
There are two points of contact – the drug store and the office/clinic. The pharmaceutical companies have had success with the former. Their drug reps know what doctors are prescribing to inform their sales calls. If a patient filled out a brief questionnaire at the drug store, I think they’d have to give consent to have that information passed on if it were by patient. I don’t know if that would apply by drug alone. But how long the patient took the medication has traditionally been an useful parameter to consider.
"What about the waiting room questionnaires? I’d much rather they ask about the medications the patient is on than being used to screen for depression. It’s really the ongoing data after a drug is in use that clinicians need anyway – more important than the RCT that gets things started…"
Nice work. Keeps it focused and keeps it simple – not too many moving parts. I am reminded of Eugene Stead’s oft-quoted advice to medicine residents: see one, do one, teach one.
Not bad.
The problem I encountered was that a lot of people can’t recall the medications and need a list prompt. Here is an old version of my current list:
http://gdpsychtech.blogspot.com/2012/03/medication-prompt-lists.html?q=medication
I present the list at the appropriate time and develop a timeline of response/nonresponse/side effects.
If there are any programmers out there – we need an app/program where a person can just select with their finger and slide that medication across the months or years that they took it. A popup of side effects at the same time would be a plus.
Most waiting room scales are review of systems of varying complexity because that allow for billing a higher E&M code.
Drug-drug interactions and polypharmacy: When did this problem start and become intolerable? Have you been treated for this problem before this prescribed treatment? What was the outcome? Is it a possibility that the problem to be helped was drug-induced? How long have you been taking the drug in question? Are you responding to the questions about being helped or having adverse effects from a regular daily record or are you recalling? What other drugs are you taking? etc
@GeorgeDawsonMD There is an app for reporting side effects, although maybe not exactly what you described. Check out MedWatcher.org. It formats and submits your adverse event report to the FDA, and lets you view side effects reported by other takers of the drug.
The questionnaire is a start. However, it misses what may be the single most important variable to ask about. And that is the sense of therapeutic alliance that the person feels to their physician. The famous TDRCP study of CBT, interpersonal therapy, imipramine, and placebo, asked participants how strong was the sense of teamwork they felt to their clinicians. Participants who felt a good sense of alliance with their clinician, and who got a placebo, showed more recovery than those who had a poor alliance with their clinician and received imipramine.
Yes, ladies and gentlemen, WHO was giving the pill was more important than whether the pill was a placebo, or imipramine. The effect of the relationship swamped whatever effect there was from the pill.
This result is no surprise to clinical psychologists, as the therapeutic alliance is the single most important predictor of progress in therapy, far stronger than the type of therapy used, experience of therapists, credentials, etc (the last three have no impact on outcome, BTW).
Research that supports this finding is available here at http://jamanetwork.com/journals/jamapsychiatry/article-abstract/494915
and at Psychother Res. 2014 May ; 24(3): 257–268.
I consider this issue to be Nobel Prize level of importance. How many other interventions exist where the alliance between patient / client and clinician is more important than the surgery / pill / injection itself?
This is whats needed as a patient who was on two different SSRIS I encountered many side effects, you should also add age and ask length of time on said drug. Plus ask what dosage their on. Plus you could give a list of side effects and ask the patient to tick any that applies to them.
I think this should be routine in every Drs surgery and patients notes and filled out or asked at every refill. That way a Dr gets to see the real picture and it makes the patient think more about the side effects their experiencing on SSRIS . I wished they had had that when I was taking them because I wasn’t even aware I was detached or the meaning of it until I came off them. Its really important to ask these very important questions to a patient who is especially in a drug induced haze and not even aware of it. SSRIS destroyed my life this could have made a very huge difference.
Please, please bring something like this out it would be life saving.
What about doing this in the process of the medical interview? I have always found paper interactions on medical history less than appealing and I don’t really pay attention and or focus on all of the historical incidents that preceded each prescription for whatever medical concern I am concerned with. That being said, I try to avoid all medical interactions because the process is so blatantly awful for both the physician and myself.
Remember true old fashioned medical exams and interviews? This takes time and actual face to face contact for more than five minutes.
Thanks for the parody of today’s medical care.
Reading through this thread reminds me that clinical interaction with a patient about medication, whether written or verbal, tries to serve 2 masters that can interact in complicated ways. Bolstering the power of positive expectation, and priming the recognition of serious adverse effects. It seems important that neither one be too much undermined by whatever questionaire one chooses to use.