 The SSRI era in psychiatry began with Prozac® in 1987 and dominated the 1990s as a steady stream of new drugs were approved by the FDA. When it became apparent that they were only effective in approximately one third of the patients, the term treatment resistant
The SSRI era in psychiatry began with Prozac® in 1987 and dominated the 1990s as a steady stream of new drugs were approved by the FDA. When it became apparent that they were only effective in approximately one third of the patients, the term treatment resistant  depression came in vogue to describe the patients who didn’t respond, and a variety of strategies were proposed to increase their effectiveness [algorithms]. One such program was the Texas Medical Alogorithm Project [TMAP] which prescribed sequencing algorithms using expensive in-patent drugs for the huge Texas Public Mental Health systems. Director Dr. John Rush then was awarded a $35 M NIMH grant to study a sequencing algorithm of antidepressants in a large cohort of subjects. It was called STAR*D.
depression came in vogue to describe the patients who didn’t respond, and a variety of strategies were proposed to increase their effectiveness [algorithms]. One such program was the Texas Medical Alogorithm Project [TMAP] which prescribed sequencing algorithms using expensive in-patent drugs for the huge Texas Public Mental Health systems. Director Dr. John Rush then was awarded a $35 M NIMH grant to study a sequencing algorithm of antidepressants in a large cohort of subjects. It was called STAR*D.
 By any criteria, this was the clinical trial from hell. The idea was to start with one antidepressant [Celexa®] and then treat nonresponders with another antidepressant, and continue for four iterations. The treatment algorithm was arbitrary. Nothing worked right and in the end, the dropout rate was so high that the results were immaterial, whatever they were. The extensive protocol called for the HDRS-17, [clinician administered] to be the primary outcome variable. Along the way, Dr. Rush developed another scale, the Quick Inventory of Depression Symptoms which came in three versions: QIDS-C [clinician rated]; the QIDS-S [a self administered version]; and the QIDS-S-telephone [a self administered version using an automated telephone call-in system].
By any criteria, this was the clinical trial from hell. The idea was to start with one antidepressant [Celexa®] and then treat nonresponders with another antidepressant, and continue for four iterations. The treatment algorithm was arbitrary. Nothing worked right and in the end, the dropout rate was so high that the results were immaterial, whatever they were. The extensive protocol called for the HDRS-17, [clinician administered] to be the primary outcome variable. Along the way, Dr. Rush developed another scale, the Quick Inventory of Depression Symptoms which came in three versions: QIDS-C [clinician rated]; the QIDS-S [a self administered version]; and the QIDS-S-telephone [a self administered version using an automated telephone call-in system]. During the study, at each visit, a staff member administered the QIDS-C, available to the clinicians treating the subjects for treatment purposes. The patient later filled out a QIDS-S for the study. And subjects filled out a QIDS-S-telephone in the follow-up groups. There were to be HDRS-17 at key end points. When the study was finally reported, the HDRS-17 data was nowhere to be found [Primary Outcome Variable]. Instead, the QIDS values were used, and as best I could tell, the various versions were lumped together. When the study was published, the authors said:
Psychometric properties of the Quick Inventory of Depressive Symptomatology [QIDS-SR] in UK primary care.
by Cameron IM, Crawford JR, Cardy AH, du Toit SW, Lawton K, Hay S, Mitchell K, Sharma S, Shivaprasad S, Winning S, and Reid IC.
Journal of Psychiatric Research. 2013 47[5]:592-598.
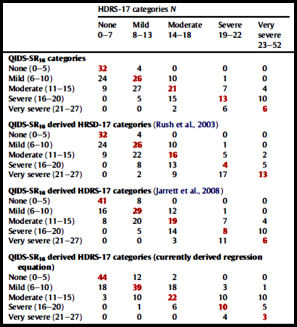
It is widely believed that severity of depressive disorder should guide treatment selection and many guidelines emphasise this factor. The Quick Inventory of Depressive Symptomatology [QID-SR16] is a self-complete measure of depression severity which includes all DSM-IV criterion symptoms for major depressive disorder. The object of this study was to assess the psychometric properties of the QIDS-SR16 in a primary care sample. Adult primary care patients completed the QIDS-SR16 and were assessed by a psychiatrist [blind to QIDS-SR16] with the 17-item Hamilton Rating Scale for Depression [GRID-HAMD]. Internal consistency, homogeneity and convergent and discriminant validity of the QIDS-SR16 were assessed. Severity cut-off scores for QIDS-SR16 were assessed for convergence with HRSD-17 cut-offs. Published methods for converting scores to HRSD-17 were also assessed. Two hundred and eighty-six patients participated: mean age = 49.5 [s.d. = 13.8], 68% female, mean HRSD-17 = 12.6 [s.d. = 7.6]. The QIDS-SR16 exhibited acceptable internal consistency [Cronbach’s alpha = 0.86], a robust factor structure indicating one underlying dimension and correlated highly with the HRSD-17 [r = 0.79] but differed significantly in how it categorised the severity of depression relative to the HRSD-17 [Wilcoxon Signed Rank Test p < 0.001]. Using published methods to convert QIDS-SR16 scores to HRSD-17 scores did not result in alignment of severity categorisation. In conclusion, psychometric properties of the QIDS-SR16 were found to be strong in terms of internal consistency, factor structure and convergent and discriminant validity. Using conventional scoring and conversion methods the scale was found not to concur with the HRSD-17 in categorising the severity of depressive symptoms.
 TMAP was shut down in disgrace and resulted in large settlements against J&J who financed the whole
TMAP was shut down in disgrace and resulted in large settlements against J&J who financed the whole scheme scam. STAR*D was mismanaged, misreported. The report here just magnifies STAR*D‘s worthlessness. Dr. Trivedi’s IMPACT study to computerize the algorithms never made it out of the gate because the doctors wouldn’t use his computers. The CO-MED study [combining antidepressants] was a decidedly negative study. And EMBARC is on its way to joining it as yet another hole in Texas into which the NIMH throws lots of money.
Yes, we can do a whole lot better than this.
Many of us are going to make sure we do.
Duane
FYI
conservative political columnist writes about DSM5
Op-Ed Columnist
Heroes of Uncertainty
By DAVID BROOKS
http://www.nytimes.com/2013/05/28/opinion/brooks-heroes-of-uncertainty.html
George Dawson, MD, DFAPA discusses Brooks column
Thursday, May 30, 2013
Brooks on Psychiatrists As “Heroes of Uncertainty”
http://real-psychiatry.blogspot.com/
jamzo,
IMO, David Brook’s piece made sense.
Dr. Dawson’s was more of the same.
“Psychiatry is to medicine as astrology is to astronomy.” – Leonard Roy Frank
Duane
here i go again cluttering up comments with FYI posts
Appreciating the politics of psychiatry
Concerns over the DSM are part of a bigger issue concerning the power of the psychological and neurological sciences
http://www.guardian.co.uk/science/political-science/2013/may/28/politics-psychiatry
STAR*D is still cited in many textbooks and clinician’s guide as a rationale for treatment, for example, see the Psychiatric Disorders section of Current Medical Diagnosis & Treatment http://www.mhprofessional.com/downloads/products/0071763724/cmdt12ch25.pdf
This stuff gets recirculated endlessly in secondary sources. It will take a long, long time for the influence of STAR*D to die.
Thanks, Dr. Mickey, for challenging the whole concept of “treatment resistant depression” — especially when “TRD” is defined as a failure to respond to SSRI’s. For many years people who do not obtain relief from SSRI’s have been told they have this unusual and much more serious condition called “TRD.” It’s been used to induce compliance with ever more punishing chemical regimens, ECT, implantable vagus nerve stimulators and god knows what other dubious and risky measures, assumed to be needed to counteract this terrible disease. It’s frightening, demoralizing, disempowering — and most importantly, there’s no basis for it. One of the embarrassing lessons of STAR-D was that “failure to respond” to SSRI’s is extremely common — enough so that any rational person would see it as discouraging news about SSRI’s rather than the “disease” they are supposed to treat.
When I failed to lose weight on the South Beach Diet a couple years ago, no one told me: OMG, you have South Beach Resistant Obesity! So I just decided South Beach wasn’t the miracle it was cracked up to be, and lost a bit of weight some other way. Thank god there was no obesity specialist on hand to sell me exotic drugs or surgery to treat my desperate case of SBRO. Ain’t exactly skinny yet, but still trying (g).
Johanna,
South Beach Resistant Obesity is a great example! I can’t wait to run into somebody who talks about TRD to counter with “SBRO“…
Thanks
And let us not overlook the contribution of drug adverse effects, prolonged withdrawal syndrome, and subsequent drug hypersensitivity to that faux phenomenon called “treatment resistant depression.” All in all, it’s probably iatrogenic!!!!
George Dawson, MD is a hero of illogic. He says
“Is psychiatry really not a science because it is complex and attempts to deal with the complicated phenomena associated with the human brain? Should we ever be concerned about 1:1 mappings of psychiatric disorders onto a specific genetic or neurobiological defect? Is it possible that a human nervous system is so complex that it is unrealistic to expect that this might happen?”
Well, yeah, it might be unrealistic. And until the system is mapped, psychiatry is merely interpreting shadows on the wall of a cave. Operating from wild counter-empirical guesses about a hugely complex system does not make psychiatry a science. If the system is beyond understanding, the fault is psychiatry’s, not the system’s.
Mickey, I’m curious about patients with what you would diagnose with melancholia, who responded very well to antidepressants (and it’s a Godsend for them), and what impact these shady trials and legacy of shady trials might have on them. What percentage of those patients respond to antidepressants on the market? Do the tricyclics work as well or better than the SSRIs? Do some melancholics not respond to any of the antidepressants that are available now? Is there a need to develop more antidepressants on behalf of this population?
Letters
Psychiatry on the Scientific Spectrum
Published: May 29, 2013
To the Editor:
Re “Heroes of Uncertainty” (column, May 28):
While I share David Brooks’s frustration over the slow progress in finding the biological causes of mental disorders, I am concerned about his opinions on the scientific basis of psychiatry and the clinical care that it provides to millions of people. The brain has proved to be infinitely more complex than any other organ in the human body, and the functions that mediate behavior are the most highly evolved in the animal kingdom.
Diagnosis is an art as well as a science, and it often represents an approximation of the true illness. Malaria was diagnosed and its symptoms were treated long before its cause was known. Autism was not described in the medical literature until 1943. Migraine and other headaches are diagnosed by symptoms, as there is no physical evidence or laboratory test.
The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders reflects the current state of our knowledge, limited as it may be. This does not negate its value in helping clinicians evaluate and treat patients, as well as the fact that it can and will continue to be improved as subsequent research enables us to better understand the biology of the brain and mental illness.
JEFFREY A. LIEBERMAN
New York, May 29, 2013
The writer is president of the American Psychiatric Association and a professor of psychiatry at Columbia University College of Physicians and Surgeons.
http://www.nytimes.com/2013/05/30/opinion/psychiatry-on-the-scientific-spectrum.html?_r=0
Wiley,
That is, in fact, a great question. I haven’t seen a huge number of those cases, and most of the ones I was involved in treating were in the years before the SSRIs. One of the main selling point for the SSRIs was their softer adverse effects profile, not their increased efficacy. The drug companies played that down [or hid it]. The people I respect in Biological Psychiatry, the ones with long experience, all say the TCAs are more effective in Melancholia. I’m pretty sure they would answer your questions “Yes.” “Yes” to tricyclics work better and “Yes” need for better drugs for these patients. Perhaps they might comment on your questions..
It brings up the topic that fills the comments whenever it’s mentioned – ECT. Patients with Melancholia unresponsive to drugs [TCAs] are the prime candidates for ECT. Whenever it’s mentioned, its opponents rise to the occasion. It wasn’t my area, but in training I treated two such patients with ECT with miraculous and immediate results. I’ll admit to being awed in spite of my skepticism. I expect we’d all welcome a pharmacologic alternative. Melancholia is often a totally showstopping and sometimes fatal illness. Not having a discrete category in the DSM-5 is outrageous.
“The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders reflects the current state of our knowledge”
“it can and will continue to be improved as subsequent research enables us to better understand the biology of the brain and mental illness.”
How it really works:
http://www.psychologytoday.com/blog/how-everyone-became-depressed/201305/the-dsm-system-how-it-really-works
The doubling down on the Fad, Fiat, and Fallacy is troubling. And how this is being purposefully promulgated by APA leadership and allowed to fester further even more so. This idea that the DSM-5 is primarily a reflection of the current state of knowledge, and of the understanding of the biology, deserves to get questioned further.
That DSM-5 primarily “reflects the current state of our knowledge,” even if one restricts this to our knowledge of “the biology of the brain and mental illness.” This appears to be accepted in many quarters, by both critics and defenders.
That is NOT how it really works.
Considered by some to be one of the most eloquent descriptions of melancholia:
William Styron’s Darkness Visible.
Even with the great diversity of views in this discussion it likely contains something that almost everyone would find of value.
Annon,
Not just a classic, Darkness Visible is the classic…
I might add some of the journals of Virginia Woolf [I’m aware that there’s great controversy over her diagnosis, but I was convinced by Kay Jamison’s work]…
Darkness Visible is available free on-line.
http://archive.org/stream/DarknessVisiblewilliamStyron/123144___william_styron_-_darkness_visible_–_a_memoir_of_madness#page/n1/mode/2up
Treatment resistance?
That’s a good thing!
A person can find something that actually works… something that is truly safe and effective.
Being “treatment resistant” is right up there with non-compliance for anyone interested in getting “weller than well!”
Duane
You questioned why the NIMH keeps pouring money into these algorithmic trials. Maybe because there’s even more money to be made in spinoffs.
Check this out:
http://www.cmeinstitute.com/psychlopedia/depression/19tdpc/sec1/section.asp
It’s J Clin Psych’s: Evaluating and Monitoring Treatment Response in Depression Using Measurement-Based Assessment and Rating Scales, by Madhukar H. Trivedi, MD.
And the QIDS features prominently.
Those of us who have to take board certification exams every 10 years also have to include in our maintenance of certification, PIP modules. These involve, for example, reviewing 5 charts of patients with a diagnosis of depression, and checking to see if you’ve implemented appropriate scales to measure improvement. Then appropriate scales are recommended, many of which can be conveniently filled out by the patient in the waiting room. Several months later, you’re supposed to assess how well you’ve implemented these forms, in order to improve quality of care. This is REQUIRED for MOC. (See http://psychpracticemd.blogspot.com/2012/11/alphabet-soup.html)
I’d bet there’s a whole market out there for novel assessment scales to be used by clinicians who are “up to standard of care”, a slew of research to be done to develop these scales, and lots of money to fund the research.
Reading Darkness Visible, I cannot relate. He talked about Camus, a writer I like, but could never relate to. The two conditions for which I was diagnosed with “depression” were nothing like this. Except for two brief episodes of mortality salience, I have never experienced such states as the author describes in this book. In the throes of my psychotic episode, when I “realized” that the human race was going to be extinct soon, and that God was going to destroy my soul over and over again for eternity (like in the sci-fi horror Event Horizon) my horror was not disembodied or divorced from experience— it was like a dream that gave shape to traumatic feelings for which the event itself was too dry and ordered to describe.
In Darkness Visible, Styron says that, ““Our perhaps understandable modern need to dull the sawtooth edges of so many of the afflictions we are heir to has lead us to banish the harsh old-fashioned words; madhouse, asylum, insanity, melancholia, lunatic, madness.”
It seems to me that getting rid of the category of Melancholia and lumping it in with so many different and disparate states, is “dulling the sawtooth blades” of melancholia. Such a grueling condition should be top priority for drug research, especially with its unbearable push toward suicide.
As much as I resent the drugs and cocktails I’ve been prescribed for a depression I never had, the thought that someone suffering from such darkness as this man describes being put through the same wringer is worse— the passage of time, or changes in circumstances or scenery would not stop the deterioration of his condition. Being in group therapy for “depression” without another melancholic soul being around sounds like a very bad joke. It’s quite an injustice that psychiatry and pharma are more concerned about expanding the market to cover people who aren’t happy than finding solutions for an oppressive disorder that has plagued the human race for ages.
Washington State still uses TMAP in fact the state hired John Chiles in 2008 http://involuntarytransformation.blogspot.com/2012/10/washington-state-hired-architect-of.html#.UaqTHUBwptE the Director of Medicaid for Washington state called TMAP a “Best Practice” in Senate Testimony in 2008. http://involuntarytransformation.blogspot.com/2012/11/tmap-is-considered-best-practice.html#.UaqTZkBwptE
… the study published in the Lancet was funded by NIMH, conducted by US researchers, but was not published in the US, and no press release was issued by NIMH.
The better to hire John A Chiles, M.D. with, my dear, to dish out those atypical anti-psychotics. What a racket.
mHealth:
“Using mobile technologies to more rapidly and accurately assess and modify behavior, biological states and contextual variables has great potential to transform medical research. Recent advances in mobile technologies and the ubiquitous nature of these technologies in daily life (e.g., smart phones, sensors) have created opportunities for research applications that were not previously possible (e.g., simultaneously assessing behavioral, physiological, and psychological states in the real world and in real-time).”
http://obssr.od.nih.gov/training_and_education/mhealth/mHealth_2013.aspx?etoc
Not sure if anyone provided the link to the recent review of Greenberg and Taylors’ books in the Los angeles Times by sociologist/historian of psychiatry Andrew Scull, but here it is:
http://lareviewofbooks.org/article.php?type=&id=1677&fulltext=1&media=#article-text-cutpoint
Dr. Noll,
Will make one more attempt at this question just in case you didn’t see it under the other post:
http://1boringoldman.com/index.php/2013/05/29/psychiatric-diseases/#comment-245394
“Imagine a world …, in which psychiatrists actually leveled with us about the limits of their knowledge. Greenberg has outlined such a thought experiment:
What would happen if [psychiatrists] told you that they don’t know what illness (if any) is causing your anxiety or depression, or agitation, and then, if they thought it was warranted, told you that there are drugs that might help (although they don’t really know why or at what cost to your brain, or whether you will be able to stop taking them if you want to; nor can they guarantee that you (or your child) won’t become obese or diabetic, or die early), and offer you a prescription [for these substances].
Psychiatry’s status is precarious enough as it is. One can only guess to what depths it might sink in such a transparent world.”
As laid out previously by Dr. Carroll there are a number of instances where the thought experiment may not apply. Rather than rearguing that, here is something that was striking: to me the experiment sounds a lot like what 1bom has described he does in clinic now.
1bom seem to have true confidence in the practice of psychiatry, in its worth, if not the current state of his field. And he seems the better psychiatrist for it.
“Psychiatry’s status is precarious enough as it is. One can only guess to what depths it might sink in such a transparent world.”
1bom does not seem to believe this. Dr. Carroll does not believe this. They so not seem to live in the shadow of psychiatry’s “precarious status.” One can wonder how many of their psychiatric colleagues do, and much worse off they are for it.
Because 1bom appears to be conducting that thought experiment in practice every week and his patients seem to keep coming back. I wonder to to make of that.
Dr. Mickey wrote: “One of the main selling point for the SSRIs was their softer adverse effects profile, not their increased efficacy. The drug companies played that down [or hid it].”
And let us not forget the “softness” of the adverse effects profile was exaggerated just as the lack of efficacy was hidden, for the sake of sales.
Richard Noll, thank you for the pointer to Andrew Scull’s review of The Book of Woe and Hippocrates Cried. A very fine article.
Note the echo in the title Delusions of Progress: Psychiatry’s Diagnostic Manual to Marcia Angell’s Delusions of Psychiatry in the NY Review of books.
Okay, so the consensus is “delusional”?
For thirty years I’ve been reading text books, articles, lectures, attended conferences about “schizophrenia”, mingling and living with people labelled so, trying to understand the whys, whats and where (in the biology of of the stigmatized, repressed, subdued, silent) of what many consider an illness of the brain. I’ve often asked experts these simpel questions. Some stare blankly, most just talk around, and around, as though they know. Until the whys and the whats are documented, I know at least that “schizophrenia” is a construct, an idea with many connotations in the heads of most professionals, without which they might feel lost and bewildered. The question of where is easily answered: On the margins of society, on the streets, in prisons, in dire straits, unless blessed with a loving and faithful family
Annonymous — just added a reply to your post on the other blog. Sorry for missing you!
Good Lord! It’s disturbing to read about psychiatrists endorsing seizures – events that make medical doctors flinch and sweat. Putting a patient into a postictal state for a couple of weeks would not strike any neurologist as a “good idea” – it’s not a matter of “clearing the circuits”, you’ve produced a total “blackout”. All of this reminds me of a tale from my graduate education: there is a frog model for myasthenia gravis and supposedly a few of these afflicted frogs sustained a leg injury necessitating amputation. Wonder of wonders, the amputee frogs showed an improvement in their myasthenia gravis symptoms. The excited researcher proclaimed, “Amputation cures myasthenia gravis”.
I take back what I said above—- the passage of time, or changes in circumstances or scenery would not stop the deterioration of his condition. Being in group therapy for “depression” without another melancholic soul being around sounds like a very bad joke.
Now that I’ve finished Darkness Visible and have read
“… the real healers were seclusion and time.”
and
“… as many as half [of}. those who are devastated once will be struck again; depression has the habit of recurrence. But most victims live through even the worst relapses, often coping better because they have become psychologically tuned by past experience to deal with the ogre. It is of great importance that those who are suffering a siege, perhaps for the first time, be told— be convinced, rather— that the illness will run its course and that they will pull through.”
And understand that he lost his mother when he was a child, I’m thinking that more effective drugs may still be useful in the most suicidal cases; but that this condition might best be handled with Open Dialogue, and the possibility of being hospitalized for the purpose of chilling out and taking a break from responsibilities before a person bottoms out in despair.
The fact that without generous insurance or wealth, a mental health vacation cannot be had without danger, nearly requires people to degenerate into madness before they can be helped. This problem has many tentacles, not the least of which are insurance, HMOs, the legal power of psychiatric diagnosis, and the stigma against being overwhelmed emotionally and psychically.
Richard Noll,
Richard Noll,
ECT is not safe.
I hope this helps. –
http://psychrights.org/Research/Digest/Electroshock/electroshock.htm
Duane
Just so you know, chemotherapy has killed people, if not directly, certainly did not enhance the quality of life the remainder of days some cancer patients lived.
So, we advocating that rather extreme measures just be abandoned so even the 20% or more who might benefit, and want to try to benefit, are denied because opponents who paint this dark, bleak picture that EVERYONE is harmed by ECT?
Do you ever let a person have the chance to talk how ECT had a positive impact on their life, they had a restoration of function and had minimal if any side effects from the procedure? I’ve been to a site in the past where a person spoke positively about ECT and then was brutally excoriated by this zealot anti-ECT crowd that paints EVERYONE as wrong and brainwashed if not echoing the extremist mind set.
It is dishonest, it is disingenuous, and it is mean to try to push this less than credible salespitch that ECT is evil. It ain’t for all, but, it ain’t for none either.
I am sure people will have a rebuttal.
ECT is the BEST treatment for melancholic depression. Period.
Darkness visible is William Styron’s best gift, I think, so I’ve passed copies on to some other sad/grieving temporarely shipwrecked persons. Styron pulled through, all the wiser, thanks most of all to his wife, I think, who did not stray from “the straight road” as he got lost in the dark woods in the middle of his journey through life. If she had not been there, to be woken up, confided in, he might have killed himself that dark night when he contemplated killing himself. Styron starts and ends by quoting Dante’s The Devine Comedy, whose women are the spiritual guides helping the traveller refind the right way, the path to a new life.
Thank you, wiley, for the exemplary retraction: “I take back what I said above.”
Dr. Noll, thank you for your response.
1BOM, Agreed, Darkness Visible is the classic of the condition of Melancholia.
I believe I can appreciate why Wiley would choose to change the absolutist tone on his original comments. Thankfully, throughout the millenia people have found ways to make it through the worst of this condition (for the great majority of that time without medication or something like ECT). Thank goodness. We are fortunate Styron survived (at least in some part so that he was present to write the work we are currently discussing). Sadly, some haven’t.
Whatever ways one chooses to try to make some sense of that condition of Melancholia (for himself he chooses at times to use the term illness), and of how people pull through, I would really hesitate to point to his writing as an example of why there should be no significant role for medication or ECT as a part of helping individuals in the throes of severe Melancholia.
I truly find it hard to believe that would have been Styron’s intent.
As far as I remember, Styron wrote about being medicated, wondering whether the drug might play a part in his descent into the abyss. He questioned dr “Gold’s perspicacity” and his Halcion medication, by Upjohn, sold as an efficatious drug, raw data of multiple negative trial data and adverse effects kept under wraps …
Perhaps someone else could clarify this further. I had not recalled that being Styron’s main assessment of his psychiatric medication regimens, which I thought he had chosen to stay on until his death. I had also thought that he had eventually chosen to utilize ECT, but would be open to correction on both counts.
To Anonymous: I know absolutely nothing about Styron’s treatment, except what I remember from reading his book several times towards the end of the last century. I no longer have copies of Darkness Visible, they were passed along as a good, wise book to be shared. I just checked the name of the medication he mentioned, which I remembered as the so-called antipsychotic Haldol, much used here then, but it was a benzo, Halcion. So I Googled Halcion, and found a familiar, checkered story.
I do not presume to know what’s right for other people, provided they are fully informed of the risks of poisonous pills. But how can people be fully informed when doctors are not, because they’ve been (have let themselves be) duped, deceived, beguiled, seduced by you know who – Big Pharma and Big Pharma money, as told by. Robert Whitaker, Ben Goldacre, David Healy, and my hero, the late Loren Mosher, his resignation letter to APA can be taken a stimulant on a grey day.
Joel,
Re: ECT – Why not start with the basics: What is it? How does it work? Has it been proven safe and effective?
Good luck, especially with the last one! –
http://breggin.com/index.php?option=com_content&task=view&id=40&Itemid=52
Nothing like having a calm debate about how brain concussions might serve the needs of a few.
Duane
Those particular questions are what will soon cause the profession to collapse, because a growing number of people are asking them, and are not pleased with the answers they are receiving.
How is it a monopoly was ever put in place with these so-called “treatments”?
How is it the profession continues to use force, carte blanche?
In the word of Ricky Ricardo, there’s “some splainin’ to do.”
Duane
The science (lack thereof) behind ECT
“‘She falls down a well, her eyes go cross. She gets kicked by a mule. They go back. I don’t know.” – Eddie, National Lampoon’s Christmas Vacation
Duane
Gee, I guess all those hospitals that allow the procedure to be done are risking all those genuine lawsuits how destructive and detrimental ECT has been for these past 4 decades or more since the technology has been refined.
Here is one point you might have that I have seen, why so many colleagues just ignore it or dismiss it as a trivial correlation is beyond me: ECT is detrimental to those who have primary Axis 2 disorders, so it is imperative in the work up the doctor tries to assess the baseline characterological factors that brings the patient in for this allegedly intractable mood disorder issue.
The memory loss and agitation post procedure is real in these patients.
But, in true Axis 1 mood disorders with pervasive suicidality, melancholia, psychosis, and profound failure to thrive, the procedure has merit.
Again, how do you expect to gain viability in just denying everyone consideration for a procedure just because some do not tolerate it? Are you ignoring my analogy with chemotherapy because it does not fit your paradigm?
ECT antagonists really have no ground in their zeal to dismiss the treatment outright. Again, polarized viewpoints don’t win arguments, see Washington DC as example A of why society is eroding with representation that really is only resentment at the end of the day.
Careful application of ECT yes, global application no. Is gray really that terrifying a concept for some who peruse these blogs?!
tell my last patient who had ECT, is getting maintenance procedures every 4-6 weeks and now back to work and maintaining independence he will have to stop because a small group in America think it barbaric and crude.
yeah, I’m sure he’ll thank you profusely!!!
Joel,
Recently, you learned about the history of your profession – its deep roots to eugenics. By your own admission, it was an eye-opening experience.
Do you know the history of electroshock (ECT)?
Really? –
http://www.endofshock.com/pig.htm
Loretta was convinced in 2006 that ECT “saved her life.”
Now, not so much.
A lot of that going on, Joel… –
http://www.madinamerica.com/2013/04/did-electroshock-save-my-life/
The other URLs (PsychRights and Dr. Breggin) have numerous links to check out.
Nothing personal here.
The facts are the facts.
Duane
But you take one example and apply it to every single doctor, I acknowledged at my site your position about eugenics had merit, but, you lose any viable point by damning the whole profession by a minority bad element.
Face it, your mentality insists that police forces should be eliminated. You are polarizing and losing any moderate, middle ground group interested in results, not just satisfying a minority interest.
And, there are plenty of holes in the Anti-ECT examples at the end of the day. That Duke doctor on one of those morning outrageous talk shows about 8-10 years ago was exposed for not presenting all the facts in trying to damn ECT. It took what was some valid points and made his presentation look narrow minded.
ECT has a place. If you are hellbent to argue eliminate it from any consideration, you are being hypocritical in not challenging other extreme medical interventions that legitimately are offered as more invasive interventions that may save lives.
Frankly, your push to insist I am wrong really makes me wonder if there is a covert agenda to basically tell people with serious mental illness they are either not ill, or have no hope. And if i am right in this interpretation, well, that is sad.
Serendipity sometimes starts with negative outcomes, but, responsible people looking for true positive and healing impacts learn from the mistakes. That has happened with ECT, and in the end, the extremists just run tape of procedures from the 1950s and claim this is the status quo.
I have seen people benefit. You won’t dismiss those experiences just because you have video or testimonials of others who it failed, and, I have the right to be skeptical if it is not floridly transparent why people are changing their tune.
Especially from internet driven propaganda. Scientology is out there, sir, and sometimes it takes a good detective to drag out the real intent.
But, thanks for offering to other readers different viewpoints.
http://m.npr.org/news/Science/187534467
Here are 3 individuals having an enormous impact on how mental illness is being defined.
Great.
Dr. Carroll should probably have a drink (or two) before listening to this broadcast.
Joel,
For the record, I’m Catholic, not a scientologist.
Please stop!
Re: Wanting to tell people they are either not ill or have no hope.
What?!
Human suffering is very real, and can at times be based upon underlying physical conditions. I’ve been clear on that point. I want to give people hope.
Real hope, not the myth of lifelong, incurable brain diseases.
When you hit, you hit hard.
But being challenged is not your strong card.
A lot of that in your profession…
Duane