Moving from left to right, first there was TMAP [1998], the PHARMA scheme originating in Texas that had seventeen States paying top dollar for psychotropic drugs instead of using the equivalent generics – finally busted by Allen Jones blowing the whistle. It was followed by STAR*D [2001], the $35 M sequencing study of antidepressants that produced hundreds of papers – none of which were the actual results of the study. IMPACTS [2003] followed, a study using computer generated algorithms for doctors in the State of Texas to follow treating depressed patients. It never got off the ground because the doctors wouldn’t follow instructions. CO-MED [2008] was something of a quickie, trying various combinations of antidepressants. Drs. Rush and Trivedi actually finished and reported that one [it was a bust].
If you’re following this, there’s a theme here – getting more out of antidepressants by following some kind of rules in the way they’re given. Except for TMAP, they’ve all been financed by the NIMH and have taken a bite out of the public money going for research. In 2008, when Senator Grassley added his name to the list being investigated, John Rush who was the leader left it to his assistant, Madhukar Trivedi, to finish things up and took off for China to head the Duke program there.
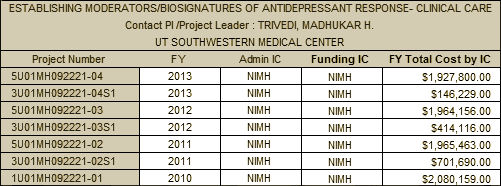
But the legacy lives on. Dr. Trivedi received an NIMH grant for yet another shot at improving the outcome of antidepressants. One might have thought that since CO-MED said that even in combination, the results aren’t better, the notion of some kind of discriminatory administration might improve things would finally die out – but hope springs eternal. And so to EMBARC [2010], an attempt to predict who will respond to which antidepressant by measuring all possible things neuro-something and locating predictors. It’s called "personalized medicine" and it was all the rage there for a while, but it’s died off in recent years. Though it may be gone from the stage, it’s not forgotten [about to go over the $10 M mark]:
- Biological psychiatry. 2013 73[2]:111-118.
- The British journal of psychiatry. 2013 203:310-301.
- Psychological medicine. 2012 42[7]:1417-1428.
- the track record above
- very poor study design
- highly unlikely base hypothesis
- switching to an SSRI that is possibly inert
That’s a heck of a cottage industry.
Not to worry.
We’ll just keep borrowing money from China:
http://www.usdebtclock.org/
Duane
And to think… we spent all this money on worthless drugs.
Plenty harmful, but worthless.
Duane
Thanks for such a brilliant piece of sharp critical thinking.
About “Skipping the step of refining what we’re treating in the first place…”
What would you suggest in order to perform such refining? I am a young psychiatrist who lives in an old Europe that has buried its refined psychopathology under tons of “neuro-something”. Psychiatrists-to-be are often taught to act as cowboys with a DSM in one hand and a Pharmacopeia in the other. Psychotherapy is “not for physicians”. Predoctoral students have to learn how to get funds in a highly competitive manner, and those in control are bureaucrats with only one thing in mind: how to carry money from public taxes to private hands. In this sense, technology is becoming an end and not a mean. They don’t care about ethics or methodology. Academic success is measured by impact factor and the editorial world has subjugated knowledge under the laws of market. Even opinion leaders are marketing experts.
Where do we start? How can we shift focus from the pockets of Pharmaindustry to the signs and symptoms of our patients and their well-being?
Christmas day was spent with family. Two young members have been working with troubled youth and they both expressed their frustration with the medicate orientation of treatment and the lack of follow through by doctors.
They identified people over medicated, and others that should be in an institution, along with the usual group of parents in denial about their child’s situation.
Each and every one of the people discussed needed more personal interaction with a trained mental health professional, not more medication. Drugs loose their effectiveness and with the addition of more drugs the resulting drug interactions only turn a treatable situation into a downward spiral that leads to even further personal and family pain.
Like the discussion taking place in general medicine, more is not always better.
Steve Lucas