by Trivedi MH, Bandelow B, Demyttenaere K, Papakosts GI, Szamosi J, Earley W, and Eriksson H.International Journal of Neuropsychopharmacology. 2013 14:1-12.
Effects of once-daily extended-release quetiapine fumarate [quetiapine XR] monotherapy on sleep quality and disturbance in patients with major depressive disorder [MDD] were evaluated. Pooled data from four 6- or 8-wk placebo-controlled quetiapine XR [50-300 mg/d] monotherapy studies [StudyD1448C00001; D1448C00002; D1448C00003; D1448C00004] were analysed. Primary efficacy end-point was change from randomization in Montgomery Åsberg Depression Rating Scale [MADRS] score. Post hoc analyses of secondary end-points were conducted for change from randomization in: MADRS item 4 [reduced sleep]; Hamilton Rating Scale for Depression [HAMD] items 4 [insomnia-early], 5 [insomnia-middle], 6 [insomnia-late] and sleep disturbance factor [items 4 + 5+6] scores; Pittsburgh Sleep Quality Index [PSQI] global scores. MADRS total score change was also evaluated in patients experiencing high and low baseline sleep disturbance [HAMD sleep disturbance factor scores >4 and <4, respectively]. In total, 1808 patients were randomized to quetiapine XR or placebo across four studies. At last assessment, quetiapine XR reduced MADRS item 4, HAMD items 4, 5 and 6, HAMD sleep disturbance factor score and PSQI global scores from baseline vs. placebo [p < 0.001]. For those experiencing high sleep disturbance [n = 865, quetiapine XR; n = 514, placebo], quetiapine XR improved MADRS total score vs. placebo at all visits [p < 0.001]. For those with low sleep disturbance [n = 252, quetiapine XR; n = 121, placebo], quetiapine XR improved MADRS total score vs. placebo at weeks 2 [p < 0.001], 4 and 6 [both p < 0.05]. In conclusion, quetiapine XR [50-300 mg/d] monotherapy improved symptoms of sleep disturbance vs. placebo in patients with MDD, including those with either high or low baseline sleep disturbance levels.
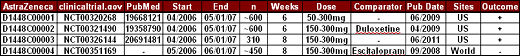
I know that my reviews of these lightweight, experimercials are boring, boring, boring. I persevere undeterred because we slept through the 1990s and most of the 2000s and let this kind of thing happen. Now here we sit in the 2010s, and my contention is that we shouldn’t let a little thing like terminal boredom stand between us and cleaning up this mess – and it is an unholy mess. This is an article about the pooled results from four studies AstraZeneca did on Seroquel XR® in MDD six or so years ago – the Moonstone Study Group. Here’s a summary of those four earlier studies:
-
Weisler RH, Montgomery SA, Earley W, Szamosi J, Lazarus A.International Clinical Psychopharmacology. 2012 27[1]:27-39.
-
Thase ME, Montgomery S, Papakostas GI, Bauer M, Trivedi MH, Svedsäter H, Locklear JC, Gustafsson U, Datto C, Eriksson H.International Clinical Psychopharmacology. 2013 28[3]:113-20.
-
Trivedi MH, Bandelow B, Demyttenaere K, Papakosts GI, Szamosi J, Earley W, Eriksson H.International Journal of Neuropsychopharmacology. 2013 14:1-12.
Dr. Madhukar Trivedi is a full Professor holding an endowed chair in Psychiatry at UT Southwestern in Dallas; he’s the Principal Investigator on a large NIMH Grant [EMBARC]; and yet he’s still signing on as a guest author to these industry funded ghost written experimercials that he really had nothing to do with. Even the STAR*D article was written by their long-time ghost-writer Jon Kilner, a Science Fiction author. Dr. Trivedi is clearly using his academic position for personal gain as a guest author and paid speaker in the PHARMA trade. When these things have been reported to his Department Chairman, Dr. Carol Tamminga, she tells us that he’s operating within the rules. I expect that the Department is getting something out of this one way or another.
And as for AstraZeneca and Seroquel® and Seroquel XR®, it’s the one that got me going on this whole pharmaceutical mess in the first place. When I started volunteering, I saw all these patients who were on Seroquel – kids and adults. It was an Atypical Antipsychotic, but the patients didn’t have psychotic illnesses. I started looking into it initially because I thought I was behind on some kind of new medical finding – thinking that there was some reason this drug was so widely prescribed. There was a reason all right – marketing:
I did a series [starts with seroquel I: introduction to an “atypical”…] and then another [starts with selling seroquel I: background…] a couple of years ago and I’ve never gotten over it. I doubt I ever will. AstraZeneca has squeezed every dollar out of a drug that’s a weak sister as an antipsychotic, riddled with sneaky dangerous side effects, and has a beguiling capacity to make people sleep. When it finally went off-patent, they had timed Seroquel XR® to keep them in the game. There was some medical finance magazine cover with smiling marketers that was praising them for their patent extension scheme. I wish I’d saved it, but it disappeared quickly – too revealing. The articles described here are simply absurd. I expect you could get these results with Valium in a CRO study of MDD if you gave enough. Even the FDA balked at approving it for monotherapy in MDD.
So why would AstraZeneca even bother to publish these pooled studies? I guess they’re milking the last drops before it goes off-patent – getting the Seroquel XR® name out there because Abilify® [the big seller these days] is also approved for MDD augmentation:
Taking a dopamine antagonist to help with major depressive disorder is like using jet fuel to put out a fire…
It matters not what a fire chief has to say, because it’s void of common sense!
Duane
Unfortunately, Seroquel is also “good to the last drop” when it comes to war-traumatized veterans. A story on the news today about this, with comments by Dr. Peter Breggin…
It’s a shame veterans are being treated this way… as if the symptoms of PTSD can be dealt with by taking mind-altering drugs. I too need to stop before I go into a rant.
Thank you for the post.
Duane
Sorry to publicise my own work but, from a population-level, Seroquel is (i) surprisingly quite widely and heavily prescribed, (ii) is curiously popular with certain subpopulations, and (iii) is generally (but particularly for these subpopulations) responsible for “rising community-level harms and greater harm relative to other atypical antipsychotics”:
(Sorry, maybe I’m not au fait with this interweb thing)
http://www.ncbi.nlm.nih.gov/pubmed/23350582
Remember this? The poster boy?
Evaluating the sleep quality of someone who took an antipsychotic before bedtime would be like measuring the blood sugar of a diabetic who ate a candy bar. In other words, I don’t know anyone who has taken an anti psychotic for sleep who felt very refreshed the next day. And of course, when the med goes south on an person and all psychotics do, it will be alot of fun getting off of the med.
Have to say, the primary villain here is still Lilly with Zyprexa, they set the standard with scum and treachery (Obi Wan to Luke in first Star Wars) that forced the other new second generation antipsychotics to keep pace with. Oh, and this term “novel” antipsychotic, what a farce!
But, AZ, J & J, Pfizer, and others did not disappoint, they stooped as low as they could go to make the sales. Nice post here Dr M.
According to AZ’s first quarter report dated 04/25/13, sales of Seroquel XR were down 15 percent in the US and down 17 percent in the rest of the world.
It will be interesting to see what AZ’s marketing department does with Trivedi’s representation regarding the effects of quetiapine XR, “quetiapine XR (50-300 mg/d) monotherapy improved symptoms of sleep disturbance vs. placebo in patients with MDD.”
I am still awaiting a response from the UT Chancellor regarding Trivedi’s extracurricular activities.
Is there any way to complain to NIMH about Trivedi’s conflict of interest issues ??
I’ll comment here as the comments on “has to stop” were closed due to derailment http://1boringoldman.com/index.php/2013/06/18/has-to-stop/
What does it take to discredit people like Trivedi and Nemeroff among their peers in psychiatry? Is there no such thing as a reputation? How can the entire field be so intellectually dishonest?
While reading a paper on Open Dialogue it occurred to me that the effectiveness of it was studied by following up on the patients, so now I have to wonder, where are the studies that follow up on patients prescribed different drugs to see if the effectiveness has been demonstrated in practice, not just in clinical trials?
How about a GIS heatmap of COI?
https://en.wikipedia.org/wiki/Geographic_information_system
Altostrata,
Here is Thomas Insel’s contact information:
Email: ti4g@nih.gov
Tel: 301-443-3673
If you do not receive a response, you can send a message to his boss via email at
francis.collins@nih.gov